pISSN : 3058-423X eISSN: 3058-4302
Open Access, Peer-reviewed

pISSN : 3058-423X eISSN: 3058-4302
Open Access, Peer-reviewed
Sangbin Jeong,SeungJong Kim,Moo Kyu Suh,Kwan Lee
10.17966/JMI.2022.27.4.63 Epub 2023 January 04
Abstract
Background: Few studies have been reported on facial herpes zoster and the risk factors for its complications.
Objective: This study aimed to investigate the clinical features and risk factors with facial herpes zoster.
Methods: We examined the medical records of 676 patients with facial herpes zoster during a 10-year-period from 2011 to 2020. We assessed the proportion of ocular complications, Ramsay-Hunt syndrome, and postherpetic neuralgia in patients with facial herpes zoster according to several clinical factors including age, sex, dermatomes, underlying disease, and time to initiate antiviral treatment.
Results: The incidence of ocular complications was significantly higher in males (Odds ratia [OR], 2.59; 95% CI, 1.26~5.32), and with involvement of ophthalmic branches of the trigeminal nerve (V1: OR, 14.28; 95% CI, 3.62~56.29; V1 inclusion: OR, 20.68; 95% CI, 7.99~53.55), underlying diseases (OR, 1.70; 95% CI, 1.08~2.68) and positive Hutchinson's sign (OR, 3.59; 95% CI, 1.72~7.49). Ramsay-Hunt syndrome was significantly correlated with involvement of VII dermatome (OR, 24.68; 95% CI, 2.97~204.75), and showed considerable significant with otalgia (OR, 3.31; 95% CI 0.98~11.22). Postherpetic neuralgia was significantly higher in those over 60 years of age (OR, 2.03; 95% CI, 1.48~2.78), ocular complications (OR, 2.28; 95% CI, 1.57~3.30), and ear involvement (OR 1.94; 95% CI 1.17~3.20).
Conclusion: These results demonstrated that facial herpes zoster was associated with ocular complications, Ramsay-Hunt syndrome, and postherpetic neuralgia. The incidence of these complications was related to risk factors such as sex, age, dermatome, underlying disease, Hutchinson's sign and otalgia. To decrease the risk of complications associated with facial herpes zoster, patients should receive appropriate antiviral therapy and interdepartmental consultations immediately.
Keywords
Facial herpes zoster Ocular complication Postherpetic neuralgia Ramsay-Hunt syndrome
Herpes zoster is caused by the reactivation of varicella-zoster virus (VZV), which belongs to the human herpesvirus family and remains latent in the sensory nerve ganglia after an earlier attack of varicella. Herpes zoster is an acute inflammatory disease common in elderly patients or patients with compromised cellular immunity, and it is characterized by radiating pain along a unilateral sensory dermatome with clustered vesicular rashes1-3. Patients with herpes zoster forms a major fraction of patients in dermatology department, since this condition can cause various complications, such as ocular complications, Ramsay Hunt syndrome, and postherpetic neuralgia during or after treatment, and also indicate prodro- mal symptoms of malignant tumors and immunodeficiency4.
In general, facial herpes zoster occurs when the virus is transported through the cranial nerves. Especially, herpes zoster ophthalmicus occurs when the ophthalmic branch of the trigeminal nerve is involved, leading to ocular compli- cations or permanent blindness5. Furthermore, Ramsay Hunt syndrome, also called herpes zoster oticus, occurs when the facial nerve (CN VII) and the vestibulocochlear nerve (CN VIII) are involved, manifested by various symptoms, including facial palsy, otalgia, hearing loss, tinnitus, vertigo, hoarseness, and dysphagia2,6-8. Postherpetic neuralgia is generally defined as continuous pain lasting for longer than one month after the development of a skin rash1,9-11 and occurs more frequently in patients aged 60 years or older, and in cases with severe pain or rash at the acute phase and herpes zoster ophthalmicus1-3,12. Since facial herpes zoster may leave neurological sequelae, rapid diagnosis and prompt initiation of treatment are most important13.
To date, several clinical studies have been reported regarding herpes zoster ophthalmicus14, Ramsay Hunt syndrome15, and postherpetic neuralgia16-18 in the Korean literature for dermatology; however, only two clinical studies have recently been published on facial herpes zoster by Suh et al.19 and Jeong et al.20.
Herein, we present a retrospective study on clinical presentations and risk factors for ocular complications, Ramsay Hunt syndrome, and postherpetic neuralgia comprising 676 patients hospitalized for facial herpes zoster in the department of dermatology at the Dongguk University Gyeongju Hospital during a 10-year period.
1. Subjects
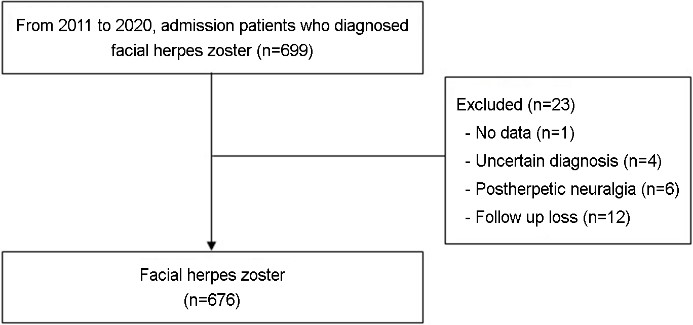
We conducted this study at the Dongguk University Gyeongju Hospital from Jan 2011 to Dec 2020. This study included patients who were hospitalized for facial herpes zoster at our department of dermatology. We excluded cases with insufficient medical records, unclear diagnosis, hospitalization for postherpetic neuralgia, and loss of follow up. All patients' electronic medical records were reviewed retrospectively. This study was approved by the Institutional Review Board of our hospital (approval No.: 110757-202103-HR-02-02).
2. Clinical characteristics
Medical records of 676 patients, who had been diagnosed with facial herpes zoster and hospitalized, were retrospectively investigated with respect to sex, age, underlying diseases, dermatome distribution, ocular complications, Ramsay Hunt syndrome, postherpetic neuralgia, initiation time of antiviral administration, and length of hospitalization.
3. Clinical classification and definition
Dermatome distribution was grouped according to the ophthalmic (V1), maxillary (V2), and mandibular (V3) branches of the trigeminal nerve, the external auditory canal and ear (VII), and the second (C2) and third (C3) cervical spinal nerves. For ocular complication analysis, dermatome involvement was classified into V1 only, V1 inclusion (V1+V2, V1+V2+V3), and V1 exclusion (V2, V2+V3). For Ramsay Hunt syndrome analysis and postherpetic neuralgia analyses, dermatome involvement was classified into V3 inclusion (V3, V2+V3, V1+V2+V3), VII, and cervical spinal nerve (C2, C3, C2+C3), and into V1, V2, V3, combination of trigeminal nerve bran- ches (V1+V2, V2+V3, V1+V2+V3), VII, and cervical spinal nerve (C2, C3, C2+C3), respectively. Ocular complications were investigated in patients whose ocular involvement was confirmed by the department of ophthalmology at the time of hospitalization, and the degree of ocular involvement was assessed every three days during hospitalization. In particular, we considered that involvement of the dermatome corres- ponding to the nasociliary branch innervating the tip or side of the nose was accompanied with Hutchinson's sign. Patients were diagnosed with Ramsay Hunt syndrome at the department of otorhinolaryngology based on vesicular rashes in the auricle and external auditory canal, otalgia, or facial nerve palsy. Finally, postherpetic neuralgia was defined when pain persisted a month after the onset of herpes zoster. Time was calculated from the initiation date of systemic antiviral administration after the onset of skin lesions.
4. Statistical analysis
Data were entered into Excel and then transferred to SPSS Version 24.0 (SPSS Inc., Chicago, USA) for analysis. Multivariable logistic regression was employed to assess the association between independent and outcome variables. We used regression diagnostic procedures to check evidence of multi collinearity or overly influential outliers in the models. All variables determined to be important (p < 0.15) were incorporated into the multivariable logistic regression analysis by stepwise methods.
1. Demographic characteristics of facial herpes zoster
Among the 699 patients who had been clinically diag- nosed as herpes zoster in the facial area and then hospitalized in the Department of Dermatology in Dongguk University Gyeongju Hospital during a 10 year period between Jan 2011 and Dec 2020, 23 patients were excluded as follows: one patient with insufficient hospitalization record; four patients with unclear diagnosis; six patients who were hospitalized due to postherpetic neuralgia; and 12 patients lost at follow up (Fig. 1). As shown in Table 1, among the 676 facial herpes zoster patients, 295 were males (43.6%) and 381 were females (56.4%), demonstrating a slight female pre- dominance (M:F = 1:1.3). Three hundred and forty patients (50.3%) were aged <60 years, while 336 (49.7%) were aged ≥60 years, with a mean age of 56.9 ± 18.3 years. Underlying diseases were confirmed in 279 patients (41.3%) as follows: 207 (30.6%) with hypertension, 82 (12.1%) with diabetes, 55 (8.1%) with both hypertension and diabetes, 28 (4.1%) with dyslipidemia, and 14 (2.1%) with malignant tumor. Regarding dermatome distribution, V1 only was most com- mon in 324 (47.9%) patients, whereas V2, V3, V1+V2, V2+ V3, V1+V2+V3, VII, C2, C3, and C2+C3 were involved in 69 (10.2%), 39 (5.8%), 14 (2.1%), 13 (1.9%), 3 (0.4%), 52 (7.7%), 20 (3.0%), 104 (15.4%), and 38 (5.6%), respectively. Dermatomes were distributed unilaterally in all 676 patients, 315 (46.6%) on the right side and 361 (53.4%) on the left side. The cases of ocular complications, Ramsay Hunt syn- drome, and postherpetic neuralgia were 184 (27.2%), 27 (4.0%), and 378 (55.9%), respectively. The time of antiviral therapy initiation was ≤4 days in 322 (47.6%) patients and >4 days in 354 (52.4%). Finally, the length of hospitalization was <7 days in 371 patients (54.9%) and ≥7 days in 305 (45.1%) (Table 1).
|
|
N |
% |
|
Sex |
|
|
|
Females |
381 |
56.4 |
|
Males |
295 |
43.6 |
|
Age |
|
|
|
<60 |
340 |
50.3 |
|
≥60 |
336 |
49.7 |
|
Age (mean ± SD) |
56.9 ± 18.3 |
|
|
Underlying disease |
|
|
|
HTN |
207 |
30.6 |
|
DM |
82 |
12.1 |
|
DM+HTN |
55 |
8.1 |
|
Dermatome |
|
|
|
V1 |
324 |
47.9 |
|
V2 |
69 |
10.2 |
|
V3 |
39 |
5.8 |
|
V1+V2 |
14 |
2.1 |
|
V2+V3 |
13 |
1.9 |
|
V1+V2+V3 |
3 |
0.4 |
|
VII |
52 |
7.7 |
|
C2 |
20 |
3.0 |
|
C3 |
104 |
15.4 |
|
C2+C3 |
38 |
5.6 |
|
Side |
|
|
|
Right |
315 |
46.6 |
|
Left |
361 |
53.4 |
|
Ocular complications |
184 |
27.2 |
|
Ramsay-Hunt syndrome |
27 |
4.0 |
|
Postherpetic neuralgia |
378 |
55.9 |
|
Time of antiviral
initiation |
|
|
|
≤4 days |
322 |
47.6 |
|
>4 days |
354 |
52.4 |
|
Length of hospitalization |
|
|
|
≤7 days |
371 |
54.9 |
|
>7 days |
305 |
45.1 |
|
HTN: hypertension, DM:
diabetes mellitus, V1: ophthalmic branch of trigeminal nerve, V2: maxillary branch of trigeminal nerve, V3: mandibular branch of trigeminal nerve, VII: facial
nerve (cranial nerve 7), C2: 2nd cervical spinal nerve, C3: 3rd
cervical spinal nerve |
||
2. Ocular complications
Ocular complications were identified in 184 (43.5%) pa- tients of the 423 with V1 or V2 involvement: 172 (53.0%) for V1 (324); 4 (5.8%) for V2 (69); 6 (42.3%) for V1+V2 (14); 1 (7.7%) for V2+V3 (13); and 1 (33.3%) for V1+V2+ V3 (3) as summarized in Table 2. The ocular complications in 184 cases comprised 90 (48.9%) patients with conjunctivitis, 63 (34.2%) with keratitis, 17 (9.2%) with uveitis, 6 (3.3%) with glaucoma, 6 (3.3%) with scleritis, and 2 (1.1%) with external ophthalmoplegia.
The statistical analysis of risk factors revealed that ocular complications occurred more frequently in males (102/195: 52.3%) than females (82/228: 36.0%) (p < 0.001), and in patients aged ≥60 (90/197; 45.7%) than <60 (94/226: 41.6%). Regarding dermatome distribution, ocular compli- cations occurred most frequently in V1 only (172/324: 53.1%), followed by V1 inclusion (V1+V2, V1+V2+V3) (7/17: 41.2%) and V1 exclusion (V2, V2+V3) (5/82: 6.1%), indicating a statistically significant difference (p < 0.001). For underlying diseases, ocular complications occurred in 51.0% (74/145) of cases: 51.1% (68/133) with hypertension, 51.9% (27/52) with diabetes, and 52.5% (21/40) with both hypertension and diabetes, showing a significantly higher frequency in patients with underlying diseases (p = 0.024). Although hypertension was associated with a higher risk of devel- oping ocular complications (p = 0.032), Bonferroni correction showed that this association was not statistically significant. Ocular complications occurred in 65.4% (34/52) of cases with Hutchinson's sign and 40.4% (59/179) of cases without Hutchinson's sign, revealing a significantly higher frequency in cases with Hutchinson's sign (p < 0.001). Finally, ocular complications occurred in 40.1% (77/192) of patients with ≤4 days of antiviral initiation, and 46.3% (107/231) of cases with >4 days, suggesting no significant difference (Table 2).
|
|
Total patients (n=423) |
p-value |
|
|
Ocular complications (+) (n=184) |
Ocular complications (-) |
||
|
Sex |
|
|
<0.001*** |
|
Female (n=228) |
82 |
146 |
|
|
Male (n=195) |
102 |
93 |
|
|
Age |
|
|
0.397 |
|
<60 (n=226) |
94 |
132 |
|
|
≥60 (n=197) |
90 |
107 |
|
|
Dermatome |
|
|
<0.001*** |
|
V1 (n=324) |
172 |
152 |
|
|
V1+V2, V1+V2+V3 (n=17) |
7 |
10 |
|
|
V2, V2+V3 (n=82) |
5 |
77 |
|
|
Underlying
disease |
|
|
0.024* |
|
Positive (n=145) |
74 |
71 |
|
|
HTN (n=133) |
68 |
65 |
0.032* |
|
DM (n=52) |
27 |
25 |
0.191 |
|
HTN+DM (n=40) |
21 |
19 |
0.228 |
|
Negative (n=278) |
110 |
168 |
|
|
Hutchinson's sign |
|
|
<0.001*** |
|
Positive (n=52) |
34 |
18 |
|
|
Negative (n=371) |
150 |
221 |
|
|
Time
of antiviral initiation |
|
|
0.199 |
|
≤4 days (n=192) |
77 |
115 |
|
|
>4 days (n=231) |
107 |
124 |
|
|
*p<0.05, ***p<0.001 |
|||
In multivariable logistic regression analysis, ocular compli- cations increased significantly with male sex (odds ratio [OR], 2.25; 95% CI, 1.45~3.47), V1 only, and V1 inclusion derma- tome (vs. V1 exclusion; V1 only: OR, 14.28; 95% CI, 3.62~ 56.29; V1 inclusion: OR, 20.68; 95% CI, 7.99~53.55), under- lying disease (OR, 1.70; 95% CI, 1.08~2.68) and Hutchinson's sign (OR, 3.59; 95% CI, 1.72~7.49) (Table 3).
|
|
Ocular complications |
p-value |
|
|
OR |
95% CI |
||
|
Sex |
|
|
|
|
Male |
2.59 |
1.26~5.32 |
0.009* |
|
Female |
1 |
|
|
|
Dermatome |
|
|
|
|
V1 |
14.28 |
3.62~56.29 |
<0.001* |
|
V1+V2, |
20.68 |
7.99~53.55 |
<0.001* |
|
V2, V2+V3 |
1 |
|
|
|
Underlying
disease |
|
|
|
|
Positive |
1.70 |
1.08~2.68 |
0.023* |
|
Negative |
1 |
|
|
|
Hutchinson's sign |
|
|
|
|
Positive |
3.59 |
1.72~7.49 |
0.001* |
|
Negative |
1 |
|
|
|
*p<0.05 |
|||
3. Ramsay Hunt Syndrome
After omitting three cases with V3 exclusion (V1, V2, or V1+V2), 269 patients with herpes zoster, whose dermatome involvement included V3 (V3, V2+V3, V1+V2+V3), VII, or cervical spinal nerves (C2, C3, C2+C3), were highly associated with auricular and periauricular involvement. As described in Table 4, Ramsay Hunt syndrome occurred in 24 (8.9%): 23 (95.8%) with VII and one (4.2%) with V3. Clinical symptoms included ear skin lesions in all 24 patients (100%), skin lesions with otalgia in 19 patients (79.2%), facial nerve involvement only without skin lesions in 19 patients (79.2%), vestibulo- cochlear nerve involvement only in three patients (12.5%), and concurrent facial and vestibulocochlear nerve involvement in two patients (8.3%).
The statistical analysis of risk factors revealed that the Ramsay Hunt syndrome occurred more frequently in males (13/108; 12.0%) than females (11/161; 6.8%), and in pa- tients aged <60 (15/123; 12.2%) than those ≥60 (9/146; 6.2%), although no statistical significance could be reached. Dermatome involvement of VII, V3, and spinal nerves was 44.2% (23/52), 1.8% (1/55) and 0%, respectively, indicating the frequent occurrence of the Ramsay Hunt syndrome with VII (p = 0.006). The Ramsay Hunt syndrome occurred in 6.3% (6/96) of cases with underlying diseases: 4.9% (4/81) of patients with hypertension, 9.4% (3/32) of patients with diabetes, and 5.9% (1/17) of patients with hypertension and diabetes. Furthermore, this condition occurred more frequently in patients with otalgia than in patients without otalgia (39.6% (19/48) vs. 2.3% (5/221)), respectively, and in patients with than without ear involvement (30.4% (24/77) vs. 0%), indicating a statistically significant difference (p < 0.001). The Ramsay Hunt syndrome occurred in 9.7% (13/134) of cases with prompt administration of antiviral agents (≤4 days) and 8.1% (11/135) of cases with delayed administration (>4 days), showing no significant difference (Table 4).
|
|
Total patients (n=269) |
p-value |
|
|
Ramsay-Hunt syndrome (+) |
Ramsay-Hunt syndrome (-) |
||
|
Sex |
|
|
0.142 |
|
Female (n=161) |
11 |
150 |
|
|
Male (n=108) |
13 |
95 |
|
|
Age |
|
|
0.084 |
|
<60 (n=123) |
15 |
108 |
|
|
≥60 (n=146) |
9 |
137 |
|
|
Dermatome |
|
|
0.006† |
|
V3, V2+V3, V1+V2+V3 (n=55) |
1 |
54 |
|
|
VII (n=52) |
23 |
29 |
|
|
C2, C3, C2+C3 (n=162) |
0 |
162 |
|
|
Underlying
disease |
|
|
0.252 |
|
Positive (n=96) |
6 |
90 |
|
|
HTN (n=81) |
4 |
77 |
0.132† |
|
DM (n=32) |
3 |
29 |
1.000† |
|
HTN+DM (n=17) |
1 |
16 |
1.000† |
|
Negative (n=173) |
18 |
155 |
|
|
Otalgia |
|
|
<0.001*** |
|
Positive (n=48) |
19 |
29 |
|
|
Negative (n=221) |
5 |
216 |
|
|
Ear involvement |
|
|
<0.001*** |
|
Positive (n=77) |
24 |
53 |
|
|
Negative (n=192) |
0 |
192 |
|
|
Periauricular
involvement |
|
|
0.313† |
|
Positive (n=10) |
0 |
10 |
|
|
Negative (n=259) |
24 |
235 |
|
|
Time
of antiviral initiation |
|
|
0.655 |
|
≤4 days (n=134) |
13 |
121 |
|
|
>4 days (n=135) |
11 |
124 |
|
|
***p<0.001, †by Fisher's exact
test |
|||
In multivariable logistic regression analysis, the Ramsay Hunt syndrome increased significantly with VII dermatome involvement (OR, 24.68; 95% CI, 2.97~204.75) and showed a considerable significance with otalgia (OR, 3.31; 95% CI, 0.98~11.22) (Table 5).
|
|
Ramsay-Hunt syndrome |
p-value |
|
|
OR |
95% CI |
||
|
Dermatome |
|
|
|
|
VII |
24.68 |
2.97~204.75 |
0.003* |
|
C2, C3, C2+C3 |
- |
- |
0.996 |
|
V3, V2+V3, V1+V2+V3 (Reference) |
1 |
|
|
|
Otalgia |
|
|
|
|
Positive |
3.31 |
0.98~11.22 |
0.054 |
|
Negative (Reference) |
1 |
|
|
|
*p<0.05 |
|||
4. Postherpetic neuralgia
Of the 676 patients with facial herpes zoster, postherpetic neuralgia occurred in 378 patients (55.9%) as shown in Table 6. The analysis of risk factors revealed that this condition was more prevalent among males (164/295; 56.2%) than females (167/214; 55.6%) and in patients aged ≥60 years (215/336; 64.0%) than those aged <60 years (163/340; 47.9%), showing a significant difference (p < 0.001). Regard- ing dermatome distribution, postherpetic neuralgia occurred in 59.3% (192/342) of V1, 50.7% (35/69) of V2, 43.6% (17/39) of V3, 56.7% (17/3) of two or more dermatomes(V1+V2, V2+V3, V1+V2+V3), 69.2% (36/52) of VII, 50.0% (81/162) of cervical spinal nerves (C2, C3, C2+C3), resulting in a descending order of occurrence, although not reaching statistical significance, as follows: VII>V1>two or more derma- tomes>V2>cervical spinal nerves>V3. Postherpetic neuralgia occurred in 61.5% (144/234) of cases with underlying dis- eases: 61.8% (128/207) with hypertension, 62.2% (51/82) with diabetes, and 63.6% (35/55) with hypertension and diabetes, suggesting a significantly higher incidence of this condition with underlying diseases (p = 0.024). Although postherpetic neuralgia was found in a greater number of patients with hypertension (p = 0.039), no statistical signifi- cance was identified after Bonferroni correction. Among 184 patients with ocular complications, 125 (67.9%) were involved with postherpetic neuralgia, showing a statistical significant trend (p < 0.001): 100.0% (6/6) of cases with glaucoma, 83.3% (5/6) of cases with scleritis, 74.6% (47/63) of cases with keratitis, 70.6% (12/17) of cases with uveitis, 60.0% (54 /90) of cases with conjunctivitis, and 50.0% (1/2) of external ophthalmoplegia, indicating higher incidence of postherpetic neuralgia in patients with conjunctivitis, keratitis, scleritis, uve- itis, and glaucoma except external ophthalmoplegia. Patients with Ramsay Hunt syndrome (18/27; 66.7%) were more fre- quently involved with postherpetic neuralgia compared to those without the syndrome (360/649; 55.5%), although not reaching statistical significance. Cases with delayed initiation of antiviral administration at >4 days were more frequently involved with postherpetic neuralgia than cases with ≤4 days, indicating a statistically significant difference (p < 0.001) (Table 6).
|
|
Total patients (n=676) |
p-value |
|
|
Postherpetic
neuralgia (+) (n=378) |
Postherpetic
neuralgia (-) (n=298) |
||
|
Sex |
|
|
0.881 |
|
Female (n=381) |
214 |
167 |
|
|
Male (n=295) |
164 |
131 |
|
|
Age |
|
|
<0.001*** |
|
<60 (n=340) |
163 |
177 |
|
|
≥60 (n=336) |
215 |
121 |
|
|
Dermatome |
|
|
0.057 |
|
V1 (n=324) |
192 |
132 |
|
|
V2 (n=69) |
35 |
34 |
|
|
V3 (n=39) |
17 |
22 |
|
|
V1+V2,
V2+V3, V1+V2+V3 (n=30) |
17 |
13 |
|
|
VII (n=52) |
36 |
16 |
|
|
C2, C3,
C2+C3 (n=162) |
81 |
81 |
|
|
Underlying disease |
|
|
0.032* |
|
Positive (n=234) |
144 |
90 |
|
|
HTN (n=207) |
128 |
79 |
0.039 |
|
DM (n=82) |
51 |
31 |
0.222 |
|
HTN+DM (n=55) |
35 |
20 |
0.229 |
|
Negative (n=442) |
234 |
208 |
|
|
Ocular complications |
|
|
<0.001*** |
|
Positive (n=184) |
125 |
59 |
|
|
Conjunctivitis
(n=90) |
54 |
36 |
<0.001†*** |
|
Keratitis (n=63) |
47 |
16 |
|
|
Scleritis (n=6) |
5 |
1 |
|
|
Uveitis (n=17) |
12 |
5 |
|
|
Glaucoma (n=6) |
6 |
0 |
|
|
Oculomotor
nerve palsy (n=2) |
1 |
1 |
|
|
Negative (n=492) |
253 |
239 |
|
|
Hutchinson's sign |
|
|
0.788 |
|
Positive
(n=52) |
30 |
22 |
|
|
Negative
(n=624) |
348 |
276 |
|
|
Ramsay-Hunt syndrome |
|
|
0.251 |
|
Positive
(n=27) |
18 |
9 |
|
|
Negative
(n=649) |
360 |
289 |
|
|
Otalgia |
|
|
0.271 |
|
Positive
(n=59) |
33 |
27 |
|
|
Negative
(n=617) |
345 |
271 |
|
|
Ear involvement |
|
|
0.133 |
|
Positive
(n=80) |
51 |
29 |
|
|
Negative
(n=596) |
327 |
269 |
|
|
Periauricular involvement |
|
|
0.316 |
|
Positive
(n=12) |
5 |
7 |
|
|
Negative
(n=664) |
373 |
291 |
|
|
Time of antiviral initiation |
|
|
<0.001*** |
|
≤4 days (n=322) |
151 |
171 |
|
|
>4 days (n=354) |
227 |
127 |
|
|
*p<0.05,
***p<0.001, †by Fisher's exact test |
|||
In multivariable logistic regression analysis, postherpetic neuralgia increased significantly with patients aged >60 years old (OR, 2.03; 95% CI, 1.448~2.78), ocular complication (OR, 2.28; 95% CI, 1.57~3.30), and ear involvement (OR, 1.94; 95% CI, 1.17~3.20) (Table 7).
|
|
Postherpetic neuralgia |
p-value |
|
|
OR |
95% CI |
||
|
Age |
|
|
|
|
≥60 |
2.03 |
1.48~2.78 |
<0.001* |
|
<60 (Reference) |
1 |
|
|
|
Ocular
complication |
|
|
|
|
Positive |
2.28 |
1.57~3.30 |
<0.001* |
|
Negative (Reference) |
1 |
|
|
|
Ear
involvement |
|
|
|
|
Positive |
1.94 |
1.17~3.20 |
0.01* |
|
Negative (Reference) |
1 |
|
|
|
*p<0.05 |
|||
Herpes zoster is an infectious dermatologic disease caused by VZV that is characterized by the manifestation of vesicular skin rashes. Although most cases are healed without specific sequelae, in some patients this disease is accompanied by neurological complications of which postherpetic neuralgia is the most common. However, in cases where the facial area is also involved, this disease may induce systemic compli- cations such as ocular complications or Ramsay Hunt syndrome21. However, to the best of our knowledge, there have only been a few studies in the Korean literature for derma- tology, such as Suh et al.19 and Jeong et al.20, investigating the effect of this disease when the entire facial area is involved. Therefore, the present study investigated the clinical pre- sentations and risk factors for ocular complications, Ramsay Hunt syndrome, and postherpetic neuralgia in 676 patients with facial herpes zoster.
Similar to the results reported by Suh et al.19 and Jeong et al.20, the frequency of herpes zoster with respect to dermatome distribution was the highest in V1 (47.9%), followed by C3 (15.4%), V2 (10.2%), VII (7.7%), V3 (5.8%), C2+C3 (5.6%), C2 (3.0%), V1+V2 (2.1%), V2+V3 (1.9%), and V1+ V2+V3 (0.4%). However, the frequency of this disease in patients with V1 innervated by the ophthalmic branch was 47.9%, which was lower than the 59.2% reported in Suh et al.19. Furthermore, this frequency in patients with VII accompanied by ear involvement and Ramsay Hunt syndrome was 7.7%, which was slightly higher than the 6.3% reported by Suh et al.19.
Ocular complications of herpes zoster include conjunctivitis, keratitis, uveitis, scleritis, glaucoma, oculomotor palsy, ptosis, retinal necrosis, and optic neuritis3,12,22-27. Male patients were found to be more susceptible to ocular complications (52.3%) than females (36.0%). Kim and Suh14, Ando and Kohmoto12 have reported that it occurred more frequently in patients over 80 years of age. Similarly, occurrence in the present study was the highest in patients over 80 years of age at 70.6%. However, there was a slight difference as shown in Jeong et al., in which the highest frequency was 83.8% for patients in their 60's. The incidence in patients aged over 60 years was 45.7% contrary to 41.6% in patients aged less than 60 years, with no statistically significant difference. In this study, V1 or V2 were involved in 43.5%, which was higher than the 22.8% reported in Suh et al.19. The ophthal- mology literature accepts that that the larger the area of the three trigeminal nerve branches, the higher the likelihood of occurrence of ocular complications28. In this study, the odds ratio was higher in V1 inclusion (multi lesion) than V1 only. According to Jeong et al.20, the occurrence of ocular complications was higher in patients with underlying diseases, such as hypertension and diabetes, but there was no statistically significant difference. In contrast, the present study confirmed that this higher incidence was statistically significant. The positive rate of Hutchinson's sign in which skin lesions occur either at the tip or side of the nose corresponding to the nasopharyngeal branch accounts for 20~70% in patients with herpes zoster ophthalmicus1. In this study, the positive rate of Hutchinson's sign was 18.5%, which was similar with the 17% reported in Ando and Kohmoto12. The incidence of ocular complications was 65.4% in patients with Hutchinson's sign, which was higher and statistically significant compared to the incidence of 40.4% without Hutchinson's sign, a finding consistent with previous studies12,22,24. Differences pertaining to the time of antiviral initiation (≤4 days and ≥4 days) were not significant. It is thought that the patients with severe ocular symptoms were hospitalized earlier. The incidence of ocular complications was higher in the patient group with hospitalization of ≥7 days than the group with ≤7 days; however, this finding may be a result of the prolonged treatment period due to the accompanying ocular complications.
Ramsay Hunt syndrome occurs when VZV invades the geniculate ganglion present in the facial and auditory nerves. This condition can cause facial palsy, tinnitus, and nystagmus accompanied by severe ear pain. Rarely, it can also cause dizziness and sensorineural hearing loss by invading the vestibular organ2. In this study, the incidence of Ramsay Hunt syndrome was 8.9%, which was slightly higher than 4.7% and 5.6% in patients with facial palsy reported in Min et al.15 and Suh et al.19, respectively. However, an accurate comparison could not be made due to the different patient groups. Dermatome distribution revealed that the VII nerve group was most commonly invaded at 85.2%, an incidence that was statistical significant and similar to the 78.2% rate shown in Suh et al.19. Regarding the clinical symptoms in patients with Ramsay Hunt syndrome, ear skin lesion was the most common symptom shown in 100% of cases, while skin lesion accompanied by otalgia was found in 79.2% of cases. The likelihood of occurrence of Ramsay Hunt syndrome was high and statistical significant in cases with a skin lesion in the ear or otalgia. Consequently, Ramsay Hunt syndrome must be suspected in such cases, and a consultation with an ENT specialist is necessary. In contrast, there was no statistically significant difference for the occurrence of Ramsay Hunt syn- drome based on the time of administration of the antiviral drug on the fourth day. This was initially thought to be due to the relatively small number of patients with Ramsay Hunt syndrome. The duration of hospitalization was significantly higher (p < 0.001) in the group with ≥7 days than in the group with ≤7 days (17.3% vs. 1.4%), but it is thought to be a result of the prolonged treatment period due to the accompanying Ramsay Hunt syndrome.
The incidence of postherpetic neuralgia is known to be high in the presence of herpes zoster ophthalmicus, severe pain, and rash in the acute phase, and in elderly patients ≥60 years of age1-3,12. By age, Jeong et al.20 reported that posther- petic neuralgia was present in 63.2% of patients aged ≥60 years old, which was similar to the incidence rate found in the present study (64.0%, p < 0.001). Furthermore, the in- cidence of postherpetic neuralgia was higher in patients with underlying diseases (61.5%). Kim and Suh14 reported that 50% of patients with ocular complications had postherpetic neuralgia, and this was reported to be 48.4% and 42.4% in Suh et al.19 and Jeong et al.20, respectively. In the present study, this incidence rate was higher (67.9%), showing a statistically significance difference. This result might be due to the difference in the patient groups; hence, further investigations with a greater number of patients will be necessary to validate these findings. In particular, considering ocular com- plications, Szeto et al.29 reported that postherpetic neuralgia was statistically significant only in uveitis (15.2%). However, in this study, postherpetic neuralgia occurred in 100% of cases with glaucoma, 83.3% of cases with scleritis, 74.6% of cases with keratitis, 70.6% of cases with uveitis, 60.0% of cases with conjunctivitis, and 50% of cases with ocular motor palsy. Moreover, the incidence of postherpetic neuralgia was high in all ocular complications except ocular motor palsy. The incidence of postherpetic neuralgia in patients with and without Ramsay Hunt syndrome was 66.7% and 55.5%, respectively, and the difference was not statistically significant. The average length of time elapsed before patients visited the hospital and started receiving antiviral treatment was 5.1 days, which was slightly different from the 4.2 days re- ported in previous studies15,16. Multivariable analysis showed no significant difference between the groups that started antiviral treatment within and after four days, suggesting that early antiviral treatment initiation did not reduce the incidence of postherpetic neuralgia. The average length of hospital stay was 6.9 days, and the incidence of postherpetic neuralgia was significantly higher among patients whose hospital stay was ≥7 days. Our findings indicate that more severe pain and skin rashes during the acute phase associated with longer hospital stay with increased incidence of postherpetic neuralgia.
This study has some limitations. First, the patient group included only inpatients, thus the number of patients with severe symptoms was relatively high. In the future, studies on more cases, including outpatients, are necessary to supplement the limitations of this study. Second, this study was conducted as a retrospective study with medical record analysis in a single institution. Therefore, the information was limited with reliance on the records. However, this study may be considered to be of great significance in that it was able to investigate the clinical features and risk factors for ocular complications, Ramsay Hunt syndrome, and postherpetic neuralgia in a patient group with facial herpes zoster comprising 676 participants.
This study was conducted retrospectively to investigate the clinical features and risk factors for ocular complications, Ramsay Hunt syndrome, and postherpetic neuralgia in 676 patients with facial herpes zoster who had been hospitalized in our dermatology department from January 2011 to December 2020.
The incidence of ocular complications was found to be higher in males than in females, in cases of dermatome V1 invasion, in the presence of comorbidities, such as hyper- tension, and in patients with a positive Hutchinson's sign. The incidence of Ramsay Hunt syndrome was higher in patients with otalgia. The incidence of postherpetic neuralgia was higher in the elderly patients (≥60 years of age), with ocular complications, and ear involvement.
In conclusion, it is necessary to analyze the related risk factors in advance to minimize potential complications and provide appropriate treatments at an early stage for patients hospitalized with facial herpes zoster. If other diseases are suspected, the respective departments should be consulted.
References
1. 1Levin MJ, Schmader KE, Oxman MN. Varicella and herpes zoster, In: Kang S, Amagai M, Brunckner AL, Enk AH, Margolis DJ, McMichael AJ, et al. editors. Fitzpatrick's dermatology in general medicine. 9th ed. New York: McGraw-Hill, 2019:3035-3064
2. Ahn HH, Huh EP, Lee UH, KIM KM, Park CJ, Ahn JY, et al. Infectious skin diseases, In: Textbook of dermatology, 7th ed. Seoul: McGraw-Hill Education Korea, 2020:367 -369
3. 3Weinberg JM. Herpes zoster: epidemiology, natural history, and common complications. J Am Acad Dermatol 2007; 57:S130-S135
Google Scholar
4. Friedman-Kien AE, Lafleur FL, Gendler E, Hennessey NP, Montagna R, Halbert S, et al. Herpes zoster: a possible early clinical sign or development of acquired immuno- deficiency syndrome in high-risk individuals. J Am Acad Dermatol 1986;14:1023-1028
Google Scholar
5. 5Becerra JC, Sieber R, Martinetti G, Costa ST, Meylan P, Bernasconi E. Infection of the central nervous system caused by varicella zoster virus reactivation: a retrospective case series study. Int J Infect Dis 2013;17:e529-e534
Google Scholar
6. Shin DH, Kim BR, Shin JE, KIM CH. Clinical manifestations in patients with herpes zoster oticus. Eur Arch Otorhino- laryngol 2016;273:1739-1743
Google Scholar
7. 7Wang F, Chen X. Case of Ramsay-Hunt syndrome associ- ated with dysphagia. J Dermatol 2011;38:1195-1197
Google Scholar
8. Ganesan V, Bandyopadhyay D, Kar SS, Choudhury C, Choudhary V. Herpes zoster infection involving mandib- ular division of trigeminal nerve and Ramsay Hunt syn- drome with meningitis in an immunocompetent patient: a rare association. J Clin Diagn Res 2016;10:OD05-OD07
Google Scholar
9. 9Kost RG, Straus SE. Postherpetic neuralgia-pathogenesis, treatment, and prevention. N Engl J Med 1996;335:32-42
Google Scholar
10. Desmond RA, Weiss HL, Arani RB, Soong SJ, Wood MJ, Fiddian PA, et al. Clinical applications for change-point analysis of herpes zoster pain. J Pain Symptom Manage 2002;23:510-516
Google Scholar
11. 11Jung BF, Johnson RW, Griffin DR, Dworkin RH. Risk factors for postherpetic neuralgia in patients with herpes zoster. Neurology 2004;62:1545-1551
Google Scholar
12. Ando K, Kohmoto H. Clinical features of herpes zoster ophthalmicus. Jpn J Clin Ophthalmol 2000;54:385-388
13. 13Kim GT, Lee SH, Sim JH, Yun SH. Clinical analysis of the treatment and prognosis of herpes zoster oticus. Korean J Otolaryngol 1997;40:996-1002
14. Kim SH, Suh MK. The clinical features of herpes zoster ophthalmicus in inpatients. Korean J Dermatol 2008;46: 1337-1343
Google Scholar
15. 15Min SW, Lee KS, Won JH, Cho SY, Huh CH, Kim BJ, et al. Clinical analysis of Ramsay Hunt syndrome. Korean J Dermatol 2007;45:1121-1126
Google Scholar
16. Song JY, Chung BS, Choi KC, Shin BS. A 5-year period clinical observation on herpes zoster and the incidence of postherpetic neuralgia (2002~2006); a comparative analysis with the historical control group of a previous study (1995~1999). Korean J Dermatol 2008;46:431-436
Google Scholar
17. 17Kim YJ. Clinical observation of postherpetic neuralgia in patients with herpes zoster. Korean J Dermatol 2001;39: 1364-1369
Google Scholar
18. Kwon SB, Kim DW, Chung SL, Lee SJ. A clinical observa- tion on acute pain and postherpetic neuralgia in patients with herpes zoster. Korean J Dermatol 2000;38:314-321
Google Scholar
19. 19Suh JH, Lee SK, Lee UH, Kim MS. Facial herpes zoster: A 15-year retrospective single-center study. Korean J Dermatol 2019;57:235-242
Google Scholar
20. Jeong HH, Oh SY, Lee HJ, Heo EP, Go JW. Clinical features and risk factors of facial herpes zoster: ocular compli- cations and postherpetic neuralgia. Korean J Dermatol 2020;58:245-253
Google Scholar
21. 21Tyring SK. Natural history of varicella zoster virus. Semin Dermatol 1992;11:211-217
22. Kim HJ, Park JS, Chung H, Jang HC. Revaluation of the Hutchinson's sign. Korean J Dermatol 2007;45:1127-1131
Google Scholar
23. 23Yoshida M, Hayasaka S, Yamada T, Yanagisawa S, Hayasaka Y, Nakamura N, et al. Ocular findings in Japanese patients with varicella-zoster virus infection. Ophthalmologica 2005;219:272-275
Google Scholar
24. Zaal MJ, Volker-Dieben HJ, D'Amaro J. Prognostic value of Hutchinson's sign in acute herpes zoster ophthalmicus. Graefe's Arch Clin Exp Ophthalmol 2003;241:187-191
Google Scholar
25. 25Park MW, Hong JS, Suh MK, Lee JI. Ophthalmoplegia in herpes zoster ophthalmicus. Korean J Dermatol 2018;56: 401-403
Google Scholar
26. Jang JW, Shin DJ, Lee SJ, Jun JB, Chung SL. Ocular motor nerve paralysis in herpes zoster ophthalmicus. Korean J Dermatol 2000;38:1280-1283
27. 27Park MJ. Herpes zoster ophthalmicus complicated by acute glaucoma. J Korean Ophth Soc 1972;13:83-85
Google Scholar
28. Lee HY, KIM SY, Jung MS. Clinical features of Korean facial herpes zoster patients. J Korean Ophthalmol Soc 2010;51:8-13
29. 29Szeto SK, Chan TC, Wong RL, Ng AL, Li EY, Zhanji V. Prevalence of ocular manifestations and visual outcomes in patients with herpes zoster ophthalmicus. Cornea 2017;36:338-342
Google Scholar
Congratulatory MessageClick here!