pISSN : 3058-423X eISSN: 3058-4302
Open Access, Peer-reviewed

pISSN : 3058-423X eISSN: 3058-4302
Open Access, Peer-reviewed
Hyun Ju Oh,Seung Ah Yoo,Marianne Isabel A. Sayo,Ji Hyun Lee
10.17966/JMI.2022.27.3.55 Epub 2022 October 05
Abstract
PATIENT CONSENT STATEMENT
The patient provided written informed consent for the publication and the use of his images.
Keywords
Primary myelofibrosis Sparganosis
Sparganosis is caused by the plerocercoid larvae of the genus Spirometra. This disease commonly presents as a solitary subcutaneous or intramuscular nodule that is slow growing, typically movable and accompanied by intermittent pruritus and tenderness. The incidence of sparganosis in Korea has decreased over the last 20 years; however, cases have been consistently reported for at least the past century1.
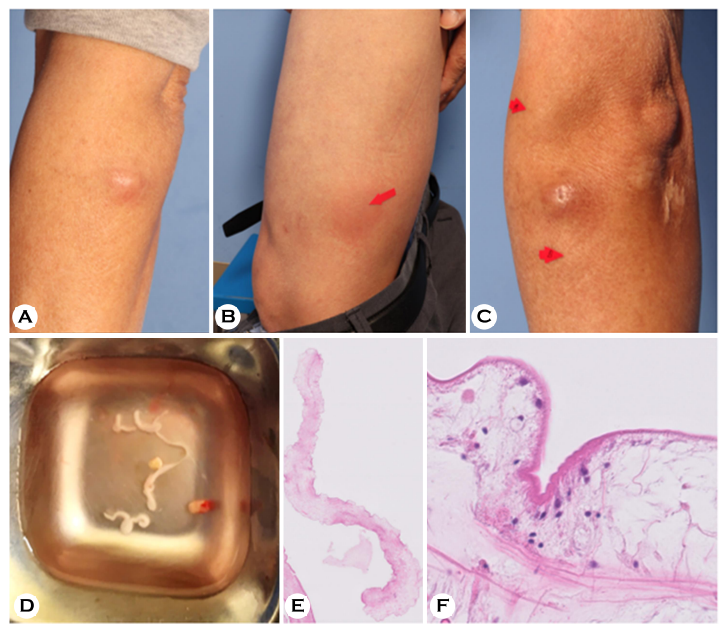
A 64-year-old man who denied exposure to infected water and consumption of raw flesh snakes or frogs, presented to our clinic with a 7-day history of having a solitary, 1.5 cm movable subdermal nodule on his left arm causing pruritis (Fig. 1A). He was previously diagnosed with primary myelo- fibrosis and was treated with allogenic peripheral blood stem cell transplantation two months prior to his consultation. He was on maintenance treatment with cyclosporine resulting in immunosuppression. Routine laboratory findings were unremarkable including the absence of eosinophilia in a peripheral blood smear.
Skin biopsy removed a long white larva-like specimen with unspecified movement in normal saline (Fig. 1D). Histo- pathological results showed calcareous bodies and muscle fibers surrounded by eosinophilic tegument in the specimen identified as a worm (Fig. 1E and F). According to the micro-scale enzyme-linked immunosorbent assay test results, the anti-sparganum specific IgG antibody level in the serum was significantly higher than the control. Based on the clinical, histological, and laboratory findings, the patient was diag- nosed with sparganosis. He was prescribed albendazole for 5 days and subsequently developed new lesions on the left arm, left leg, and both inguinal areas which were documented at the time of his 2-week follow-up visit (Fig. 1B and C). Computerized tomography detected multiple, ill-defined soft tissue masses with fat infiltration at the subcutaneous layer, and all of them were subsequently removed surgically.
Previous reports of sparganosis have verified the effects of immunosuppressive therapy to the onset of sparganosis2. Other reports have also found the absence of eosinophilia, presumably related to the immunosuppressive state of the patient. This indicates that the normal predictive value of eosinophilia on blood tests is unlikely to be present in patients with immunosuppression cases of multiple sparganosis which has been most frequently reported in immunocompromised patients. This underscores the importance of not only sus- pecting a parasitic infection in immunocompromised patients with a movable mass, but also taking all necessary steps to avoid the parasite from disseminating throughout the body including close observation.
References
1. Yoon HS, Jeon BJ, Park BY. Multiple sparganosis in an immunosuppressed patient. Arch Plast Surg 2013;40: 479-481
Google Scholar
2. Kim JG, Ahn CS, Sohn WM, Nawa Y, Kong Y. Human sparganosis in Korea. J Korean Med Sci 2018;33:e273
Google Scholar
Congratulatory MessageClick here!