pISSN : 3058-423X eISSN: 3058-4302
Open Access, Peer-reviewed

pISSN : 3058-423X eISSN: 3058-4302
Open Access, Peer-reviewed
Hyun-Min Seo,Se Kwang Park,Ji Hun Park,Ki Yeon Kim,Joung Soo Kim
10.17966/JMI.2022.27.1.21 Epub 2022 April 02
Abstract
PATIENT CONSENT STATEMENT: The patient provided written informed consent for the publication and the use of her images.
Keywords
Kerion celsi Scarring alopecia Tinea capitis
Kerion is a severe form of tinea capitis caused by an overactive immune response to infection. Kerion is distinguished by an inflammatory plaque characterized by pustules, thick crusting, and/or drainage. The initial symptom could be sup- purative folliculitis1.
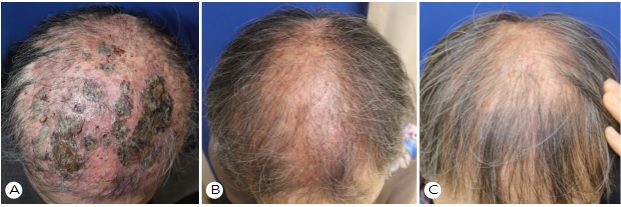
A 63-year-old female presented with diffuse painful crusted plaques on the scalp, as well as multiple inflammatory erythemas. She did not have any systemic illness or lymphade- nopathy. She presented with a three-month-old local erythematous plaque, and her condition was misdiagnosed as seborrheic dermatitis and treated with topical corticosteroids for two months in other hospitals. Despite this treatment, the lesion became wider and developed pustules and crusts (Fig. 1A). She had a cat and reported no baldness in the cat.
Hyphae were discovered in KOH performed on the scalp, as well as yellow-green fluorescence under a wood lamp. The patient was diagnosed with kerion celsi because of these findings. For six months, the patient was treated with itraconazole 200 mg/day, sertaconazole shampoo, and topical clotrimazole. An intramuscular injection of triamcinolone 40 mg/ml was also prescribed. After six months, the erythema, crust, and pustules resolved, but all the hairs did not regrow in the inflamed vertex area (Fig. 1B). Complete recovery was not achieved at the six-month follow-up, with residual scarring alopecia (Fig. 1C).
Kerion is caused by T. mentagrophytes, T. verrucosum, T. rosaceum (T. megninii), T. tonsurans, T. violaceum, and T. soudanense. Tinea capitis is caused by M. canis and M. gypseum. Such an infection is usually observed as an ordinary squamous lesion, but it can develop into kerion1.
Zoophilic dermatophytes such as M. canis, T. mentagrophytes, and T. verrucosum historically have been the most common pathogens causing kerion celsi. Over the past few decades, T. tonsurans has emerged as a major cause, especially in urban areas2.
Kerion causes scarring alopecia if diagnosis and treatment are delayed. Rivka et al.3 discovered that 27.5 percent of 80 pediatric patients with kerion celsi had cicatricial alopecia. The pathogen, antifungal treatment, duration of treatment, or use of prednisone or antibiotics did not affect the outcomes.
Kerion appears most commonly in children aged 5 to 10 and is rare in adults4.
Our case was a middle-aged woman with infection probably transmitted from a cat and that was subsequently exacerbated by topical steroid application. Clinicians should have a high suspicion index for fungal infections when dealing with inflammatory scalp lesions. Treatment should be commenced early to prevent scarring alopecia and psychological distress.
References
1. Isa-Isa R, Arenas R, Isa M. Inflammatory tinea capitis: kerion, dermatophytic granuloma, and mycetoma. Clin Dermatol 2010;28:133-136
Google Scholar
2. Lapergola G, Breda L, Chiesa PL, Mohn A, Giannini C. Kerion celsi caused by Trichophyton tonsurans in a child. Lancet Infect Dis 2018;18:812
Google Scholar
3. Friedland R, Sabbah F, Reiss-Huss S, Ben Amitai D. Epidemiologic features and risk of scarring in pediatric patients with kerion celsi. Pediatr Dermatol 2022;doi: 10.1111/pde.14916
Google Scholar
4. Zaraa I, Hawilo A, Aounallah A, Trojjet S, El Euch D, Mokni M, et al. Inflammatory tinea capitis: a 12-year study and a review of the literature. Mycoses 2013;56:110-116
Google Scholar
Congratulatory MessageClick here!