pISSN : 3058-423X eISSN: 3058-4302
Open Access, Peer-reviewed

pISSN : 3058-423X eISSN: 3058-4302
Open Access, Peer-reviewed
Jin Park,Jae-Hui Nam,Ji Hyun Lee,Joonsoo Park,Je-Ho Mun,Yang Won Lee,Jong Soo Choi,Moo Kyu Suh,Kwang Ho Kim,Weon Ju Lee,Jee-Bum Lee,Hyun Chang Ko,Hyojin Kim
10.17966/JMI.2018.23.2.33 Epub 2018 June 30
Abstract
Background: There have been several therapeutic guidelines for onychomycosis in different countries and advances in its diagnosis and treatment. Optimal treatment decision-making is affected by healthcare systems and cultural backgrounds of countries.
Objective: The executive committee for onychomycosis guideline of the Korean Society for Medical Mycology aims to provide up-to-date practical guidelines for onychomycosis management in Koreans.
Methods: The committee thoroughly reviewed relevant literature and previous guidelines. The structured algorithmic guideline was developed by experts' consensus.
Results: The optimal treatments can be selected alone or in combination based on the nail and patient variables. Three major classes of treatment are available: standard (topical or oral antifungals), additional (nail removal), and alternative treatments (laser). Both topical and oral antifungals alone are appropriate for mild onychomycosis, while oral antifungals are primarily recommended for moderate-to-severe cases if not contraindicated. Combined topical and oral antifungals are recommended to increase the efficacy in moderate-to-severe cases. Additional infected nail removal is also considered for moderate-to-severe onychomycosis, which is unresponsive to standard medical treatment alone. Laser therapy can be an alternative without significant side effects when standard medical treatments cannot be applied regardless of onychomycosis severity. After treatment course completion, periodic therapeutic response monitoring and onychomycosis preventive measures should be rendered to reduce recurrence.
Conclusion: The Korean consensus guideline provides evidence-based recommendations to promote good outcomes of onychomycosis. The proposed algorithm is simple and easy to comprehend, allowing clinicians to facilitate optimal treatment decision-making for onychomycosis in clinical practice.
Keywords
Diagnosis Guideline Onychomycosis Treatment
Onychomycosis, a fungal nail infection, is caused by mainly dermatophytes, yeasts, and non-dermatophyte molds. It is the most common nail disease that accounts for about 50% of all nail dystrophy causes and affects up to 14% of the population with an increasing prevalence among old individuals1,2. In Korea, onychomycosis is prevalent, affecting 10% of all dermatologic outpatients3,4. According to data from the National Health Insurance Service of Korea in 2015, at least 1.2 million patients with onychomycosis are being treated at a medical institution annually, and the actual number of patients is estimated to be much higher. Its prevalence is expected to increase owing to the increase in the elderly population, prevalence of systemic diseases, such as diabetes, and immunosuppressant use. Onychomycosis can cause nail disfigurement, such as discoloration, thickening, and fragility; pain; walking difficulty; and emotional embarrassment; thus, it significantly impacts patient's quality of life. It can also transmit infection to other nails and body parts and may spread to other individuals. Therefore, although onychomycosis is not life-threatening, it should be managed to improve not only patient's quality of life but also public health.
However, onychomycosis is notoriously difficult to treat. Its general treatment modalities include medical (oral and topical antifungals) and non-medical treatments or a combination of these. Antifungals, the mainstay of onychomycosis therapy, have a high ex-vivo bioavailability, but demonstrate a relatively lower cure rate, protracted treatment duration, and higher recurrence when treating onychomycosis than other superficial fungal infections. The variable clinical presentations and causative fungal species of onychomycosis and the limitation in antifungal use according to patients' health status also hinder successful treatment outcomes. Especially in Korea, many patients are reluctant in using antifungals to treat onychomycosis owing to fear of serious side effects. Instead, they attempt anecdotal treatment, such as fork remedies, without proper medical consultation to physicians. To achieve successful treatment outcomes, clinical practice guidelines should be established and utilized to assist practitioner and patient decisions regarding appropriate healthcare for specific clinical circumstances.
To date, several clinical therapeutic onychomycosis guidelines have been suggested by working groups in various countries5-10. In 1996, the American Academy of Dermatology's guideline/outcomes committee developed guidelines of care for onychomycosis for professionals5. In 2003, Roberts et al.6 published onychomycosis treatment guidelines with identification of the strength of evidence on behalf of the British Association of Dermatologists. Thereafter, the International Consensus Guideline was developed through a workshop involving experts and key opinion leaders to define an algorithm to facilitate treatment decision-making in onychomycosis7. In 2014, the British Association of Dermatologists released updated guidelines for onychomycosis management, in which the evidence level and recommendation strength were implemented8. In 2016, a simple algorithm of onychomycosis guideline was proposed by an expert panel for a Canadian treatment strategy, which reflects the current pharmaceutical options available in Canada9. However, there are differences in the disease epidemiology, individual preference to treatment method of physicians or patients, healthcare systems, and cultural backgrounds among countries, which can affect the treatment decision-making of physicians and patients. In Korea, the Korean Taskforce on Onychomycosis Education (K-TOE), comprising convened experts with knowledge and clinical experience in medical mycology, released an onychomycosis guide book for dermatologists at clinics and residents to provide insight into its diagnosis and management in 2006. The K-TOE published the second edition, expanding their previous work to provide an up-to-date onychomycosis review in 2009. In the revised edition, they suggested Korean consensus treatment guidelines through a panel discussion according to the International Consensus Guideline in 200511. In the guideline, treatment options (topical, oral, and surgical treatments) can be selected alone or in combination by the clinical criteria, such as the number of involved nail, known drug interaction, clinical subtype, causative fungal species, and suboptimal drug penetration. Although it contains detailed information on onychomycosis, including treatment regimens for Koreans based on information from the literature and personal knowledge and experience, it is rather complex and obscure to make proper treatment decisions in clinical practice. Since the publication of the previous Korean onychomycosis guideline in 2009, there has been a growing need for an update based on new clinical evidence. Indeed, there have been several advances in onychomycosis management, new diagnostics, and therapies.
The executive committee for onychomycosis guideline of the Korean Society for Medical Mycology (KSMM) aims to provide up-to-date evidence- and experience-based practical guidelines on onychomycosis management for Koreans.
1. Expert panel
For the development of the Korean onychomycosis guideline, the executive committee for onychomycosis guideline of the KSMM comprised convened onychomycosis experts nation- wide. The entire development period was 1 year (February 2017 to February 2018). Five board-certified dermatologists (Jae-Hui Nam, Je-Ho Mun, Joonsoo Park, Jin Park, and Ji Hyun Lee) served as a working group and conducted a comprehensive review of the following: 1) epidemiology; 2) diagnosis and prevention; 3) systemic treatment; 4) topical treatment; and 5) non-medical treatment (surgery and laser therapy). Eight experienced dermatologists (Hyun Chang Ko, Kwang Ho Kim, Hyojin Kim, Moo Kyu Suh, Yang Won Lee, Weon Ju Lee, Jee-Bum Lee, and Jong Soo Choi) supervised the collaborative process as the advisory group. The guideline development process is briefly summarized in Table 1.
|
1) Searching and collecting source
for guideline, and data analyses (randomized controlled trials, systematic literature
reviews, meta-analyses, previous guidelines) |
|
2) Allocation
of sections; and selection of key questions and core issues in sections |
|
3) Assessment
of evidence level on the issues; and writing draft guidelines in sections |
|
4) Algorithm
development following a full discussion based on draft guidelines |
|
5) Revision
of draft guidelines through a detailed discussion among the advisory group |
|
6) Completion
of the final guideline and determination of future plan for revision |
2. Database and literature search
In the guideline development, we used the hybrid method that combined adaptation of previous reliable guidelines and de novo development. The database and literature search sources were MEDLINE, PUBMED, Cochrane Library, EMBASE, and Google scholar. To reflect the data of the Korean onychomycosis, the KoreaMed, KMbase, National Assembly Library of Korea, and RISS were also used. The following key words were used: onychomycosis (onychomycosis, fungal infection, nail, dermatophyte, diagnosis, treatment, antifungal agent, laser, and surgery) and guidelines (guideline, consensus, and recommendation). The languages were limited to English and Korean. Although the publication date was not restricted, only those published before 2000 were included when they contained crucial information related to onychomycosis. When there were recent related systematic literature reviews and meta-analyses, those with lower evidence levels and case reports were excluded.
3. Consensus process
The collected literature was thoroughly reviewed and selected on the basis of the key questions and core issues through consensus of the working members. After the review process of the eligible literature, the evidence level for the key questions and core issues was determined, and the draft in each section was written to serve as the basis of the guideline. Following a full discussion based on the draft, the algorithm guideline was developed through consensus among the working members. Although the evidence of issue was weak, if it was clinically meaningful and consistent among all working members, it was included in the guideline. In contrast, the contents that are still on debate or far from the Korean medical situation were excluded in this guideline. The drafted algorithm guideline was revised through a detailed discussion and voting process of the advisory group. For the external review, the revised guideline was presented at the KSMM workshop involving experts, and the final version was completed through a feedback process.
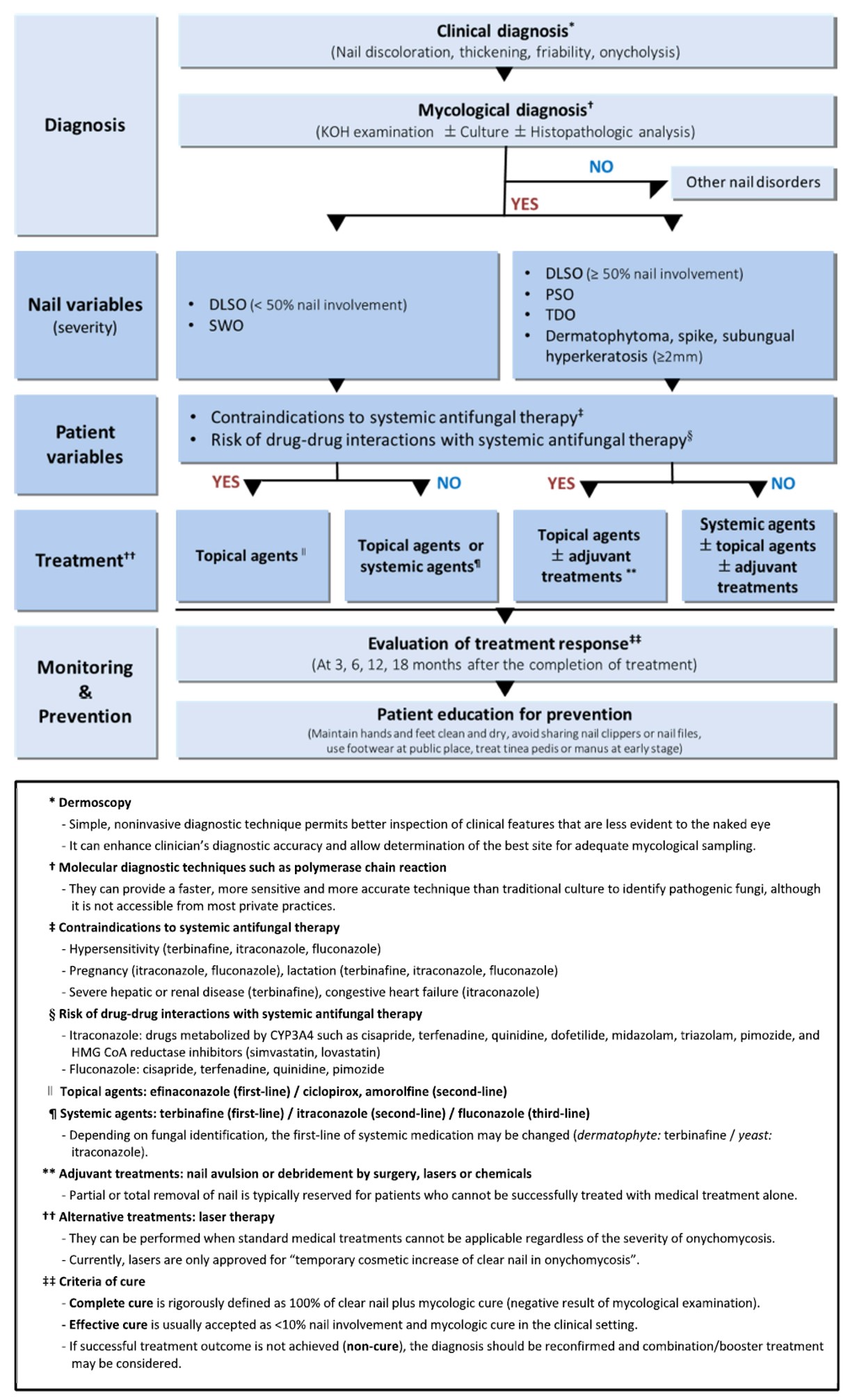
The guideline delineates diagnosis (methods and diagnostic criteria), treatment (methods, drug priority, and single or combination use), and monitoring and prevention (follow-up period, cure criteria, and preventive measures). The proposed algorithm for diagnosis and treatment of onychomycosis is illustrated with a footnote in Figure 1.
1. Diagnosis
In Korea, many patients with onychomycosis tend to visit a pharmacist or treat themselves without the appropriate diagnosis and treatment by physicians. Even some physicians instituted to treat onychomycosis based on clinical diagnosis alone. However, before starting antifungal treatment, onychomycosis should be confirmed to avoid unnecessary treatment. Onychomycosis typically presents as yellow or white discolorations of the nail plates, nail thickening, fragile nails, and onycholysis, which is highly suggestive of onychomycosis. The presence of these clinical signs can be considered as clinical criteria of onychomycosis. Simple and noninvasive dermoscopy can enhance clinicians' diagnostic accuracy of onychomycosis and allow determination of the best site for adequate mycological sampling12-14. However, its clinical signs are often difficult to distinguish from those of other nail disorders of non-fungal causes, which may lead to misdiagnosis15. Therefore, mycological examination should be used to confirm clinical suspicion of onychomycosis and rule out other nail dystrophy of non-fungal causes. Several laboratory tests are available for confirming onychomycosis, including potassium hydroxide (KOH) examination, histologic examination with nail clipping, fungal culture, and molecular diagnostic test. Among them, the simplest KOH examination, which is avail- able in almost all dermatology clinics, is recommended as a basic diagnostic technique for confirming onychomycosis. Fungal culture, histological examination with nail clipping, and molecular tests can additionally be used to increase the diagnostic accuracy or identify causative fungal species if available1,16-18. The modern molecular technique, such as polymerase chain reaction, can provide a faster, more sensitive, and more accurate assessment than the traditional culture in identifying pathogenic fungi, although it is only currently available in specialized hospital settings19,20. When a mycological test result is negative for several times, other nail disorders should be considered.
2. Treatment
For optimal treatment according to patients' status, nail and patient variables that may influence treatment choice should be identified through history taking and physical examination, and laboratory examination in selected patients after confirming onychomycosis.
1) Nail variables
There is no clear standard classification system in terms of onychomycosis severity that may have a significant effect on treatment choice. Although a few authors have suggested a numeric scoring system to assess onychomycosis severity21,22, it is rather complex and impractical in clinical settings. For these reasons, we classified onychomycosis severity into mild and moderate to severe according to simple morphological parameters (clinical subtypes, extent of nail involvement, and nail thickness), which can be discernible by naked eye examination in this guideline. This classification system allows practitioners to have a quick judgement of onychomycosis grading.
Clinical patterns were classified into distal and lateral subungual onychomycosis (DLSO), superficial white onychomycosis (SWO), proximal subungual onychomycosis (PSO), and total dystrophic onychomycosis (TDO) according to Baran's classification in 199723, except for the rare endonyx subtype. SWO with restricted superficial nail plate invasion is associated with better therapeutic responses; it is regarded as mild. Conversely, PSO and TDO involving the nail matrix of the proximal portion or entire nail, respectively, are categorized as severe because they are associated with poor therapeutic responses. DLSO, the most common form of onychomycosis, was split into the mild and moderate-to-severe types depending on the extent of nail involvement (<50% or ≥50%). Additionally, the other clinical variants associated with poor treatment outcomes, such as dermatophytoma, spike, and subungual hyperkeratosis (≥2 mm), were classified as severe regardless of the extent of nail involvement. In sum, the current onychomycosis guideline suggests a treatment algorithm for mild onychomycosis versus moderate-to-severe onychomycosis (Figure 2).
Conversely, the nail growth rate, number of affected nails, and accompanying fungal infection of other body parts are also excluded as the major variables as these do not seem to be a necessity determinant in selecting treatment modalities under the agreement of the working members.
2) Patient variables
Patients' health status and drug-to-drug interactions can affect the treatment choice, especially standard systemic antifungals. Oral antifungal agents should be avoided or administered with caution in patients with known hypersensitivity to the drugs, pregnancy, lactation, and medical illness such as severe hepatic or renal disease, congestive heart failure. In addition, co-administration of variety of drugs is contraindicated to oral antifungals, especially in azoles1,2,24,25 (Table 2).
|
Oral antifungals |
Contraindications and cautions |
|
Terbinafine |
•Hypersensitivity to terbinafine |
|
|
•Lactation |
|
|
•Severe hepatic or renal disease |
|
Itraconazole |
•Hypersensitivity to itraconazole |
|
|
•Pregnancy or lactation |
|
|
•Congestive heart failure |
|
|
•Drugs metabolized by CYP3A4 |
|
|
- HMG CoA reductase inhibitors (simvastatin and
lovastatin) |
|
|
- Hypnotic-sedative drug (midazolam, triazolam, and
pimozide) |
|
|
- Gastroprokinetic agent (cisapride) |
|
|
- Antiarrhythmic drug (disopyramide, quinidine, and
dofetilide) |
|
|
- Calcium channel blocker (bepridil, felodipine, and
lercanidipine) |
|
|
- Antihistamine (astemizole and terfenadine) |
|
Fluconazole |
•Hypersensitivity to fluconazole |
|
|
•Pregnancy or lactation |
|
|
•Drugs metabolized by CYP3A4 |
|
|
- Hypnotic-sedative drug (midazolam, triazolam, and
pimozide) |
|
|
- Gastroprokinetic agent (cisapride) |
|
|
- Antiarrhythmic drug (disopyramide, quinidine, and
dofetilide) |
|
|
- Antihistamine (astemizole and terfenadine) |
Patients' characteristics, such as age, sex, adherence to drugs, and geographical and socioeconomic status, were excluded as patient variables of this guideline because they do not seem to be essential factors in determining treatment modalities.
3) Choice of treatment methods
There are three major classes of onychomycosis treatment: (1) standard (topical or oral antifungals), (2) additional (adjuvant; nail removal), and (3) alternative treatments (laser or photodynamic therapy). The optimal onychomycosis treatment can be selected alone or in combination based on the nail and patient variables. This guideline covers only drugs, interventions, and surgeries, which are currently performed or approved in Korea, and describes a priority rating of drugs for practical guidance for clinicians. The priority of antifungals was determined in the order of the highest efficacy based on the evidence from the available literature review results. The priorities may be readjusted by additional studies and introduction of new antifungals.
(1) Standard treatment
The standard treatment of onychomycosis is topical and systemic antifungals, which are the only method of eradicating causative fungi. Unless it is contraindicated (Table 2), oral antifungals are considered the gold standard option for treating onychomycosis because of the highest cure rates and shorter treatment period regardless of onychomycosis severity. In Korea, the currently available oral antifungals include terbinafine, itraconazole, and fluconazole. Among these, terbinafine is the first-line drug owing to its fungicidal action and highest clinical and mycological cure rates, especially in dermatophyte onychomycosis26-31. Itraconazole is also effective in treating onychomycosis, but has a lower cure rate and higher risk of drug interactions than terbinafine; thus, it is regarded as the second alternative26-28,32-34. Nevertheless, itraconazole demonstrates better treatment outcomes in onychomycosis caused by yeast (candida species) and some non-dermatophyte molds and is considered as the drug of choice in these cases32,33. Fluconazole is recommended as the third option for patients who cannot tolerate or fail to respond to terbinafine or itraconazole owing to its lowest efficacy and longer treatment period26-28,35. As a general rule, children may receive the same therapy with oral antifungals as adults do; however, the dosage should be adjusted according to body weight and age1,2,36.
Generally, topical agents have fewer side effects and drug interactions than systemic agents; thus, they have their own clinical value despite their low efficacy37-39. Newer topical agents enhance nail penetration, adherence, and clinical and mycological cure40,41. Topical antifungals alone can be administered as the first-line treatment for patients with mild or moderate-to-severe onychomycosis who have contraindications to oral antifungals. Additionally, topical antifungals in combination with oral antifungals can enhance the efficacy and shorten the treatment period42,43. Amorolfine 5% nail lacquer, ciclopirox 8% solution, and efinaconazole 10% solution are currently available in Korea. Although high-quality head-to-head comparative studies are lacking, systematic literature reviews and meta-analyses indicated that efinaconazole yielded the highest clinical and mycological cure rates and is considered the first-line topical agent, followed by amorolfine and ciclopirox28,38. Meanwhile, topical antifungal lotion, cream, and ointment, which are approved for skin fungal infection treatment, are generally not recommended for onychomycosis owing to the insufficient nail penetration and lack of efficacy.
(2) Additional treatment
Additional (adjunctive) treatment involves partial or total removal of the infected nail (avulsion or debridement). Mechanical or chemical nail removal by surgery, ablative laser, or urea cream is not proven to eradicate nail fungi. Therefore, nail removal alone is not recommended as a standard onychomycosis treatment. However, when it was used in combination with conventional antifungals, nail removal increased the cure rate and patient satisfaction compared with antifungal treatment alone. Therefore, it can be a useful additional treatment option in selected cases, such as TDO, dermatophytoma, spikes, and subungual hyperkeratosis44-46. Total infected nail removal before standard medical treatment can be a more efficient strategy in patients with thickened nail based on personal experience; however, there is a lack of evidence on the issue.
(3) Alternative treatment
Alternative treatment includes laser or light therapy, which can be conducted without significant complications in patients who are difficult or reluctant to be treated with standard antifungals regardless of onychomycosis severity. This method may be particularly useful in older patients, immunocompromised individuals, and patients with hepatic impairment. Lasers are currently approved by the FDA to promote clear nails temporarily and do not address the antifungal requirements of an effective onychomycosis treatment. Among the various lasers, long-pulsed 1,064-nm Nd:YAG laser or diode laser is the most widely used type in treating onychomycosis47-49. In Korea, 1,064-nm Nd:YAG laser with a millisecond pulse duration and 405- and 635-nm combined laser have been approved as a safe and effective method for improving clinical nail presentation in patients with onychomycosis who cannot take oral antifungals based on the New Health Technology Assessment findings at the time the report was prepared. Although uncontrolled and nonrandomized laser studies show preliminary evidence of variable clinical improvements, they do not appear to have mycological cure that equates to standard medical treatment47,48. Additionally, the action mechanism and optimal regimens (number of treatments, treatment schedule, wavelength, and pulse duration) are yet to be defined. Further well-designed randomized controlled trials are necessary to consolidate the role of laser therapy for onychomycosis treatment. Photodynamic therapy is generally not recommended owing to its low cure rates, enduring pretreatment process, and treatment length compared with laser systems49-51. Folk medicine popularly used in Korea, including chemical products or cosmetics containing glacial acetic acid, pyroligneous liquid, and tea tree oil, should not be used for onychomycosis treatment because of the lack of efficacy and high risk of side or even adverse effects.
Some examples of optimal treatment strategy for individual patient conditions are as follows. For patients with mild onychomycosis (DLSO <50%, SWO), topical or oral antifungals alone are recommended as the first-line treatment. Either topical or systemic antifungals can be selected depending on the patients' preferences, number of involved nails, medication cost, and treatment duration, unless oral antifungals are contraindicated. If there is a contraindication to such, topical antifungals are administered. For moderate-to-severe onychomycosis (DLSO ≥50%, PSO, TDO, dermatophytoma, spikes, and subungual hyperkeratosis ≥2 mm), oral antifungals are considered as the first-line treatment. In recalcitrant variants of onychomycosis, topical antifungals or nail removal can be additionally used in combination with oral antifungals. However, even those with moderate-to-severe onychomycosis who are contraindicated for oral antifungals owing to underlying medical conditions or drug-to-drug interactions could be primarily treated with topical antifungals combined with nail removal. Regardless of onychomycosis severity, alternative laser therapy can be performed if patients are unable or unwilling to take medications for several reasons.
3. Therapeutic monitoring and prevention
1) Treatment
Many patients discontinue their medical treatment before they are cured, and therapy withdrawal is a major cause of treatment failure. Therefore, periodic follow-up and treatment response evaluation should be performed to achieve successful outcomes. To date, there is no definite criterion of the proper follow-up period and cure of onychomycosis52. Considering that the fingernail and toenail take 4~6 months and 12~18 months to replace a diseased nail plate, respectively, it is recommended to perform periodic follow-up monitoring with physical and mycological examinations to evaluate the treatment response after 3, 6, 12, and 18 months (endpoint: 6 months for the fingernails, 18 months for the toenails). Complete cure is rigorously defined as 100% clear nail plus mycologic cure (negative mycological examination result). However, permanent nail deformities may persist as a sequela of long-standing nail infection after elimination of the fungal pathogen despite infection resolution. Therefore, effective cure is usually accepted as <10% of nail involvement without dermatophytoma, spikes, and subungual hyperkeratosis with mycologic cure in the clinical setting. If successful treatment outcomes are not achieved (uncured), the diagnosis should be reconfirmed, and combination/booster treatment may be considered (53).
2) Prevention
Onychomycosis may recur in some patients after therapy discontinuation, with the reported rate ranging 20~50%54,55. Therefore, even if the treatment is successful, it is necessary to identify the high risk factors of onychomycosis (family history of onychomycosis, diabetes, peripheral vascular disease, immunocompromised state, and accompanying tinea manus and pedis) and educate patients regarding preventive measures to reduce recurrence (Table 3).
|
1) Maintain
clean, dry hands and feet |
|
2) Change
shoes regularly and keep drying the inside of shoes |
|
3) Do not
share nail clippers and nail care products |
|
4) Be
careful not to hurt oneself when clipping nails |
|
5) Use
private shoes and socks, if possible, in a public place |
|
6) Do not share
foot towels, slippers, and bath mats |
|
7) When
tinea pedis or manus is suspected, go to the hospital and treat it as early
as possible |
The guideline was unable to cover every occasion in practice, and adherence to these recommendations will not ensure successful treatment in every situation. The ultimate treatment decision should be made by physicians based on their knowledge and experience in view of all situations presented by patients with onychomycosis. Additionally, the recommendations of this guideline are not absolute criteria for onychomycosis treatment. Therefore, this guideline should not be used to judge adequacy of the medical practice by the law and cost.
This guideline bears several limitations. First, most of the reliable data underpinning the guideline were based on literature from western countries owing to the paucity of Korean studies on onychomycosis. Second, there may be a limitation in the development process of the guideline in terms of methodology, since the guideline was predominantly created by voluntary participation of dermatologists in the KSMM. Third, this guideline also could not provide the solution for some challenging issue of onychomycosis in the clinical setting (i.e., detailed information of boosters or supplemental therapy and follow-up treatment method in cases of primary treatment failure) owing to the insufficient evidence. It is expected that the amendments will complement the contents and systematize the development process of the guideline, thus expanding the information and reinforcing the evidence.
This guideline will be renewed by accumulation of new evidence according to upcoming publications as new diagnostic and therapeutic methods are developed; however, the specific period of revision is not mentioned herein.
The executive committee for onychomycosis guideline of the KSMM established up-to-date practical guidelines for onychomycosis management in Koreans by an expert consensus. This guideline provides evidence-based recommendations to promote good treatment outcomes of onychomycosis. The proposed algorithm is simple and easy to comprehend, allowing clinicians to facilitate optimal treatment decision-making for onychomycosis in clinical practice. While adapting previous guidelines, it contains the latest updated information on onychomycosis management. It faithfully reflects the healthcare system, patient and physician preferences, and epidemiological characteristics in Korea. We hope that this new guideline will serve as the standard for clinicians and patients on the topic of onychomycosis, thus improving patient's quality of life and public health in Korea.
In relation to this article, I declare that there is no conflict of interest.
References
1. Schieke SM, Garg A. Superficial fungal infection. In: Goldsmith LA, Katz SI, Gilchrest BA, Paller AS, Leffell DJ, Wolff K, editors. Fitzpatrick's dermatology in general medicine. 8th ed. New York: McGraw-Hill, 2012:2277 -2297
Crossref
2. Thomas J, Jacobson GA, Narkowicz CK, Peterson GM, Burnet H, Sharpe C. Toenail onychomycosis: an important global disease burden. J Clin Pharm Ther 2010;35:497 -519
Crossref
Google Scholar
PubMed
3. Yoo JY, Suh MK, Ha GY, Kim H. A clinical and mycological study of onychomycosis in the elderly over 10 years (2001-2010). Korean J Med Mycol 2014;19:83-92
Crossref
Google Scholar
4. Hwang SM, Kim DM, Suh MK, Kwon KS, Kim KH, Ro BI, et al. Epidemiologic survey of onychomycosis in Koreans: Multicenter study. Korean J Med Mycol 2011;16:35-43
Crossref
Google Scholar
5. Drake LY, Dinehart SM, Farmer ER, Goltz RW, Graham GF, Hordinsky MK, et al. Guidelines of care for superficial mycotic infections of the skin: onychomycosis. Guidelines /Outcomes Committee. American Academy of Dermatology. J Am Acad Dermatol 1996;34:116-121
Crossref
Google Scholar
6. Roberts DT, Taylor WD, Boyle J. British Association of Der- matologists. Guidelines for treatment of onychomycosis. Br J Dermatol 2003;148:402-410
Crossref
Google Scholar
PubMed
7. Lecha M, Effendy I, Feuilhade de Chauvin M, Di Chiacchio N, Baran R. Taskforce on Onychomycosis Education. Treat- ment options - development of consensus guidelines. J Eur Acad Dermatol Venereol 2005;19(Suppl. 1):25-33
Crossref
Google Scholar
8. Ameen M, Lear JT, Madan V, Mohd Mustapa MF, Richardson M. British Association of Dermatologists' guidelines for the management of onychomycosis 2014. Br J Dermatol 2014;171:937-958
Crossref
PubMed
9. Gupta AK, Sibbald RG, Andriessen A, Belley R, Boroditsky A, Botros M, et al. Toenail onychomycosis-A Canadian approach with a new transungual treatment: develop- ment of a clinical pathway. J Cutan Med Surg 2015;19: 440-449
Crossref
Google Scholar
10. Vlahovic TC, Joseph WS, Scher RK, Tosti A, Plasencia J, Pariser DM, et al. Diagnosis and management of onychomycosis perspectives from a joint podiatric medicine-dermatology roundtable. J Am Podiatr Med Assoc 2016; 106:155-162
Crossref
Google Scholar
11. Korean Taskforce on Onychomycosis Education (K-TOE). Onychomycosis; guidebook for dermatologists at clinic and residents, 2nd ed. Seoul: Seoheung Co., 2008
Crossref
12. Piraccini BM, Balestri R, Starace M, Rech G. Nail digital dermoscopy (onychoscopy) in the diagnosis of onychomycosis. J Eur Acad Dermatol Venereol 2013;27:509-513
Crossref
Google Scholar
PubMed
13. El-Hoshy KH, Abdel Hay RM, El-Sherif RH, Salah Eldin M, Moussa MF. Nail dermoscopy is a helpful tool in the diagnosis of onychomycosis: A case control study. Eur J Dermatol 2015;25:494-495
Crossref
Google Scholar
PubMed
14. Park J. Dermoscopy of superficial dermatomycosis. Korean J Med Mycol 2017;22:53-61
Crossref
15. Kim WJ, Song M, Kim HS, Kim SH, Ko HC, Kim BS, et al. Various nail disorders misdiagnosed and treated as onychomycosis. Korean J Dermatol 2011;49:408-414
Crossref
Google Scholar
16. Weinberg JM, Koestenblatt EK, Tutrone WD, Tishler HR, Najarian L. Comparison of diagnostic methods in the evaluation of onychomycosis. J Am Acad Dermatol 2003; 49:193-197
Crossref
Google Scholar
PubMed
17. Velasquez-Agudelo V, Cardona-Arias JA. Meta-analysis of the utility of culture, biopsy, and direct KOH examination for the diagnosis of onychomycosis. BMC Infect Dis 2017; 17:166
Crossref
Google Scholar
PubMed
18. Jung MY, Shim JH, Lee JH, Lee JH, Yang JM, Lee DY, et al. Comparison of diagnostic methods for onychomycosis, and proposal of a diagnostic algorithm. Clin Exp Dermatol 2015;40:479-484
Crossref
Google Scholar
PubMed
19. Petinataud D, Berger S, Contet-Audonneau N, Machouart M. Molecular diagnosis of onychomycosis. J Mycol Med 2014;24:287-295
Crossref
PubMed
20. Kim JG, Shin DH, Choi JS, Lee CH. Clinical usefulness of PCR-REBA for diagnosis of onychomycosis. Korean J Med Mycol 2017;22:62-72
Crossref
Google Scholar
21. Carney C, Tosti A, Daniel R, Scher R, Rich P, DeCoster J, et al. A new classification system for grading the severity of onychomycosis: Onychomycosis severity index. Arch Dermatol 2011;147:1277-1282
Crossref
Google Scholar
22. Sergeev AY, Gupta AK, Sergeev YV. The Scoring Clinical Index for Onychomycosis (SCIO Index). Skin Therapy Lett 2002;7(Suppl. 1):6-7
Crossref
Google Scholar
PubMed
23. Hay RJ, Baran R. Onychomycosis: a proposed revision of the clinical classification. J Am Acad Dermatol 2011;65: 1219-1227
Crossref
Google Scholar
PubMed
24. Rosen T, Stein Gold LF. Antifungal drugs for onychomycosis: efficacy, safety, and mechanisms of action. Semin Cutan Med Surg 2016;35:S51-S55
Crossref
Google Scholar
PubMed
25. Kim HJ, Park SH, Kim KH. Systemic antifungal drugs for onychomycosis. Korean J Med Mycol 2016;21:105-110
Crossref
Google Scholar
26. de Sá DC, Lamas AP, Tosti A. Oral therapy for onychomycosis: an evidence-based review. Am J Clin Dermatol 2014;15:17-36
Crossref
Google Scholar
PubMed
27. Gupta AK, Ryder JE, Johnson AM. Cumulative meta-analysis of systemic antifungal agents for the treatment of onychomycosis. Br J Dermatol 2004;150:537-544
Crossref
Google Scholar
PubMed
28. Gupta AK, Daigle D, Foley KA. Network meta-analysis of onychomycosis treatments. Skin Appendage Disord 2015; 1:74-81
Crossref
Google Scholar
PubMed
29. Sigurgeirsson B, Billstein S, Rantanen T, Ruzicka T, di Fonzo E, Vermeer BJ, et al. L.I.ON. Study: Efficacy and tolerability of continuous terbinafine (Lamisil) compared to intermittent itraconazole in the treatment of toenail onychomycosis. Lamisil vs. Itraconazole in Onychomycosis. Br J Dermatol 1999;141(Suppl. 56):5-14
Crossref
Google Scholar
30. Sigurgeirsson B, Olafsson JH, Steinsson JB, Paul C, Billstein S, Evans EG. Long-term effectiveness of treatment with terbinafine vs itraconazole in onychomycosis: a 5-year blinded prospective follow-up study. Arch Dermatol 2002; 138:353-357
Crossref
Google Scholar
PubMed
31. Lee KH, Chun SI, Cho BK, Ahn KJ, Jun JB, Park KB, et al. Efficacy of oral terbinafine in the treatment of onychomycosis. Korean J Dermatol 1993;31:567-580
Crossref
Google Scholar
32. Gupta AK, De Doncker P, Haneke E. Itraconazole pulse therapy for the treatment of Candida onychomycosis. J Eur Acad Dermatol Venereol 2001;15:112-115
Crossref
Google Scholar
PubMed
33. Gupta AK, Gregurek-Novak T, Konnikov N, Lynde CW, Hofstader S, Summerbell RC. Itraconazole and terbinafine treatment of some nondermatophyte molds causing onychomycosis of the toes and a review of the literature. J Cutan Med Surg 2001;5:206-210
Crossref
Google Scholar
34. Kim JA, Youn JI, Kim YH, Jun JB, Park KB, Lee MH, et al. Therapeutic efficacy of orally administered itraconazole in onychomycosis. Korean J Dermatol 1992;30:508-518
Crossref
Google Scholar
35. Scher RK, Breneman D, Rich P, Savin RC, Feingold DS, Konnikov N, et al. Once-weekly fluconazole (150, 300, or 450 mg) in the treatment of distal subungual onychomycosis of the toenail. J Am Acad Dermatol 1998;8:S77 -S86
Crossref
Google Scholar
36. Gupta AK, Paquet M. Systemic antifungals to treat onychomycosis in children: a systematic review. Pediatr Dermatol 2013;30:294-302
Crossref
Google Scholar
37. Murdan S. Drug delivery to the nail following topical application. Int J Pharm 2002;236:1-26
Crossref
Google Scholar
PubMed
38. Gupta AK, Daigle D, Foley KA. Topical therapy for toenail onychomycosis: an evidence-based review. Am J Clin Dermatol 2014;15:489-502
Crossref
Google Scholar
PubMed
39. Lee JH, Lee YW. Topical treatment of onychomycosis. Korean J Med Mycol 2016;21:27-33
Crossref
40. Baran R, Tosti A, Hartmane I, Altmeyer P, Hercogova J, Koudelkova V, et al. An innovative water-soluble biopolymer improves efficacy of ciclopirox nail lacquer in the management of onychomycosis. J Eur Acad Dermatol Venereol 2009;23:773-781
Crossref
Google Scholar
41. Elewski BE, Rich P, Pollak R, Pariser DM, Watanabe S, Senda H, et al. Efinaconazole 10% solution in the treatment of toenail onychomycosis: Two phase III multicenter, randomized, double-blind studies. J Am Acad Dermatol 2013;68:600-608
Crossref
Google Scholar
42. Feng X, Xiong X, Ran Y. Efficacy and tolerability of amorolfine 5% nail lacquer in combination with systemic antifungal agents for onychomycosis: A meta-analysis and systematic review. Dermatol Ther 2017;30:e12457
Crossref
Google Scholar
43. Gupta AK, and the Onychomycosis Combination Therapy Study Group. Ciclopirox topical solution, 8% combined with oral terbinafine to treat onychomycosis: a randomized, evaluator-blinded study. J Drugs Dermatol 2005; 4:481-485
Crossref
Google Scholar
44. Gupta AK, Paquet M, Simpson FC. Therapies for the treatment of onychomycosis. Clin Dermatol 2013;31:544- 554
Crossref
PubMed
45. Grover C, Bansal S, Nanda S, Reddy BS, Kumar V. Combination of surgical avulsion and topical therapy for single nail onychomycosis: a randomized controlled trial. Br J Dermatol 2007;157:364-368
Crossref
Google Scholar
46. Tietz HJ, Hay R, Querner S, Delcker A, Kurka P, Merk HF. Efficacy of 4 weeks topical bifonazole treatment for onychomycosis after nail ablation with 40% urea: a double¬blind, randomized, placebo-controlled multicenter study. Mycoses 2013;56:414-421
Crossref
Google Scholar
47. Francuzik W, Fritz K, Salavastru C. Laser therapies for onychomycosis - critical evaluation of methods and effeciveness. J Eur Acad Dermatol Venereol 2016;30:936-942
Crossref
Google Scholar
48. Gupta AK, Versteeg SG. A critical review of improvement rates for laser therapy used to treat toenail onychomycosis. J Eur Acad Dermatol Venereol 2017;31:1111-1118
Crossref
Google Scholar
49. Nam JH, Kim JY. Laser and light sources in the treatment of onychomycosis. Korean J Med Mycol 2017;22:87-97
Crossref
50. Sotiriou E, Koussidou-Eremonti T, Chaidemenos G, Apalla Z, Ioannides D. Photodynamic therapy for distal and lateral subungual toenail onychomycosis caused by Trichophyton rubrum: Preliminary results of a single-centre open trial. Acta Derm Venereol 2010;90:216-217
Crossref
Google Scholar
51. Figueiredo Souza L, Souza S, Botelho A. Randomized controlled trial comparing photodynamic therapy based on methylene blue dye and fluconazole for toenail onychomycosis. Dermatol Ther 2014;27:43-47
Crossref
Google Scholar
52. Scher RK, Tavakkol A, Sigurgeirsson B, Hay RJ, Joseph WS, Tosti A, et al. Onychomycosis: diagnosis and definition of cure. J Am Acad Dermatol 2007;56:939-944
Crossref
Google Scholar
PubMed
53. Ko HC, Kim WI. Increasing therapeutic efficacy for onychomycosis. Korean J Med Mycol 2016;21:59-64
Crossref
54. Piraccini BM, Sisti A, Tosti A. Long-term follow-up of toenail onychomycosis caused by dermatophytes after successful treatment with systemic antifungal agents. J Am Acad Dermatol 2010;62:411-414
Crossref
Google Scholar
55. Suh MK. Treatment and prophylaxis of onychomycosis. Korean J Med Mycol 2001;6:140-142
Crossref
Google Scholar
Congratulatory MessageClick here!