pISSN : 3058-423X eISSN: 3058-4302
Open Access, Peer-reviewed

pISSN : 3058-423X eISSN: 3058-4302
Open Access, Peer-reviewed
Barnali Chowdhury,Osung Kwon,Hyungrok Kim,Hyunjung Kwon,Kyungduck Park,Hyun Chung,Joonsoo Park
http://dx.doi.org/10.17966/KJMM.2016.21.4.135 Epub 2016 December 27
Abstract
Keywords
Endotrix Favus Fungal infection Tinea capitis
Tinea capitis is a common fungal infection found in school going children worldwide prevalently caused by Trichophyton and Microsporum species[1],[2]. Inflammatory lesions usually present as kerion or favus, whereas non inflammatory lesions present as black dots or grey patches. Diagnosis is usually made clinically or by potassium hydroxide mount[4]. Misdiagnosis and treatment with systemic steroids can aggravate the lesions. Herein we present a case of tinea capitis which was initially treated as psoriasis with local and systemic steroids at local clinic due to negative KOH test and diagnosed at our center by histopathology.
A six-year-old girl child presented with patchy hair loss over the scalp for one year. Initially, the lesion started as a solitary coin sized hairless patch on the left frontal area of the scalp associated with mild scales and pruritus. KOH test was done at a local clinic and was negative. The patient was given intermittent topical and systemic steroid therapy at different clinics with a diagnosis of scalp psoriasis. The lesions had been slowly aggravated as hair became brittle and it involved almost the entire scalp.
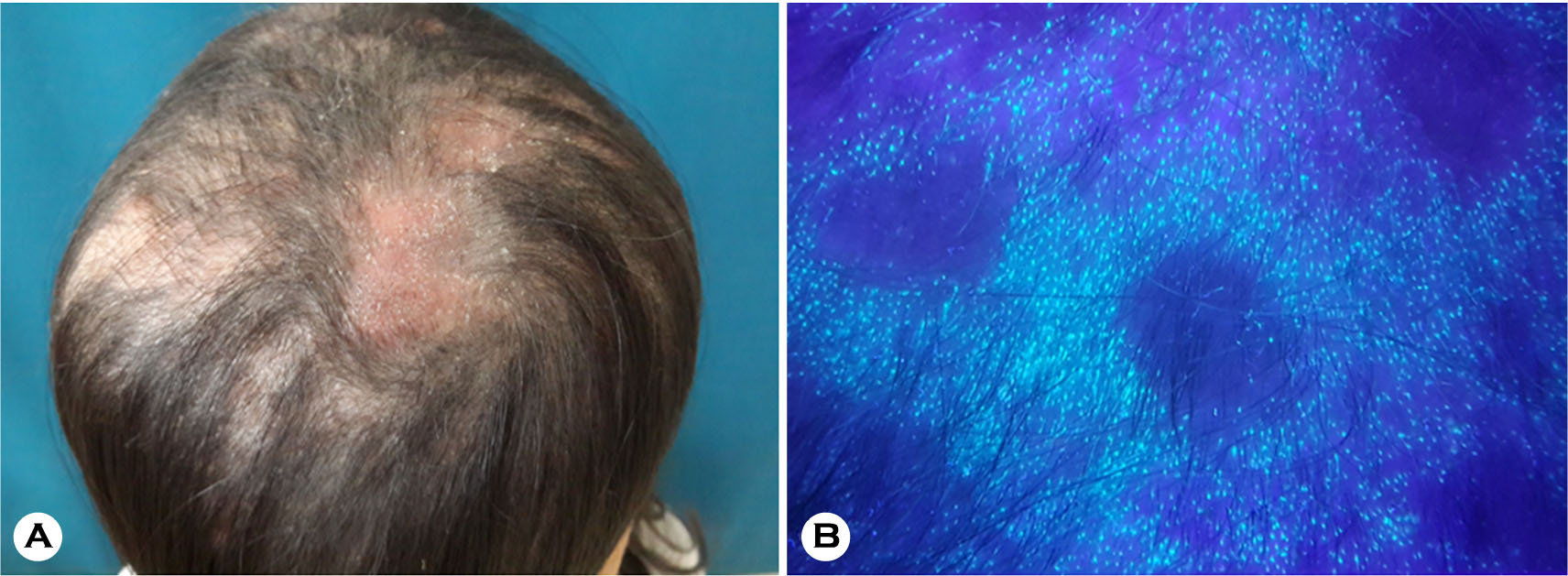
The patient visited our hospital in April 2016 for further evaluation and treatment. Dermatological examination revealed multiple bean to coin sized scaly hairless patches over the scalp (Fig. 1). There were no signs of regional lymphadenopathy and Wood's lamp examination showed greenish fluorescence (Fig. 1).
KOH test and fungal culture in Sabouraud agar medium were both negative. Laboratory investigation was nonspecific besides mild leukocytosis (11,200/μL). The patient then had undergone skin biopsy to find innumerable fungal hyphae and spores within the ectotrix, endotrix and suppurative inflammation in dermis (Fig. 2). The patient was diagnosed with tinea capitis and was started on fluconazole. The patient has been showing signs of improvement with antifungal therapy.
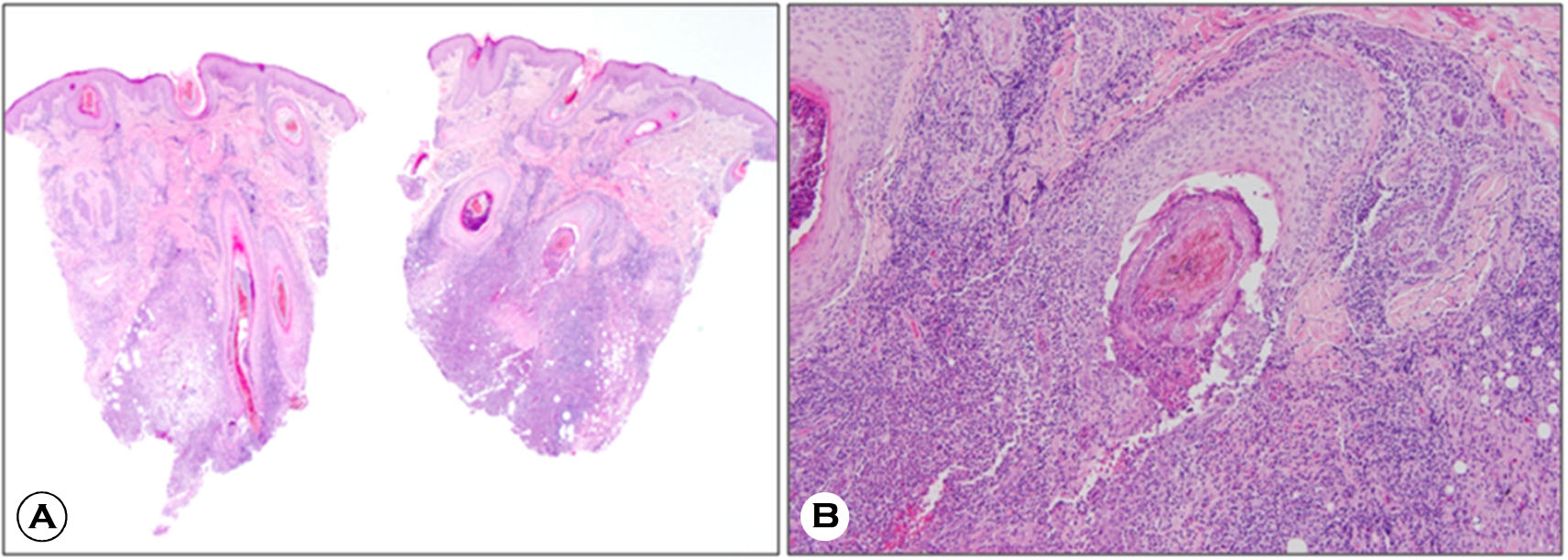
Tinea capitis is a dermatophyte infection prevalently caused by Trichophyton and Microsporum and seen commonly in children aged between 5 and 10 years[1],[3]. Three types of hair involvement have been described in tinea capitis known as ectothrix, endothrix or both depending on its level of hair involvement. Since its presentation may mimic that of other hair diseases, such as seborrheic dermatitis, atopic eczema, psoriasis, alopecia areata and ringworm of the head, history with appropriate diagnostic measures must be thoroughly identified. Diagnosis is usually made by 10~20% potassium hydroxide (KOH) test or culture of the selected hair samples. Wood's lamp examination may be conducive in ectrothrix hair involvement and culture provides precise identification of the species. Histo pathology is usually required in atypical presen-tation or unresponsiveness to treatment[5]. In addition, fungal hyphae can be demonstrated using routine Haematoxylin and Eosin stain. PAS with diastase digestion facilitates identification of fungal elements[6].
In our case, the lesions were misdiagnosed probably due to negative KOH test as steroids were started without confirming the diagnosis. The lesions had worsened as it involved the entire scalp with hair brittleness. Histopathology was ultimately conducive in making the diagnosis and the patient has shown clinical improvement upon antifungal medication. Typical diagnostic methods regarded as the gold standard, the sensitivities for KOH test and culture are 73.3% (95% CI: 66.3 to 79.5%) and 41.7% (34.6 to 49.1%), respectively[7]. Therefore it is important not to limit measure of examination to only these modalities but to further evaluate the lesion with histopathology. Recently the fungal phytopathogens can be identified via a direct acquisition of MALDI-TOF mass spectra e.g. from infected plant organs contaminated by fungal spores[8].
Despite a number diagnostic methods proposed, there is no single method that guarantees sensitivity or specificity level of 100%. Therefore a meticulous approach combined with various diagnostic measures should be taken in consideration in confirming fungal infections, thus providing the appropriate care to the patients.
Conflict of interest
In relation to this article, I declare that there is no conflict of interest.
References
1. Mirmirani P, Tucker LY. Epidemiologic trends in pediatric tinea capitis: a population-based study from Kaiser Permanente Northern California. J Am Acad Dermatol 2013;69:916-21
Crossref
Google Scholar
2. Hogewoning A, Amoah A, Bavinck JN, Boakye D, Yazdanbakhsh M, Adegnika A, et al. Skin diseases among schoolchildren in Ghana, Gabon, and Rwanda. Int J Dermatol 2013;52:589-600
Crossref
Google Scholar
3. Fulgence KK, Abibatou K, Vincent D, Henriette V, Etienne AK, Kiki-Barro PC, et al. Tinea capitis in schoolchildren in southern Ivory Coast. Int J Dermatol 2013;52:456-460
Crossref
Google Scholar
4. Fuller LC, Child FJ, Midgley G, Higgins EM. Diag nosis and management of scalp ringworm. BMJ 2003;326:539-541
Google Scholar
5. Seebacher C, Bouchara JP, Mignon B. Updates on the epidemiology of dermatophyte infections. Mycopathologia 2008;166:335-352
Crossref
Google Scholar
6. Trovato MJ, Schwartz RA, Janniger CK. Tinea capitis: current concepts in clinical practice. Cutis 2006;77: 93-99
Google Scholar
7. Levitt JO, Levitt BH, Akhavan A, Yanofsky H. The sensitivity and specificity of potassium hydroxide smear and fungal culture relative to clinical assessment in the evaluation of tinea pedis: a pooled analysis. Dermatol Res Pract 2010;2010:764-843
Crossref
Google Scholar
8. Chalupová J, Raus M, Sedlářová M, Sebela M. Identification of fungal microorganisms by MALDITOF mass spectrometry. Biotechnol Adv 2013;32: 230-241
Crossref
Google Scholar