pISSN : 3058-423X eISSN: 3058-4302
Open Access, Peer-reviewed

pISSN : 3058-423X eISSN: 3058-4302
Open Access, Peer-reviewed
Young Chae Lee,Tae Young Han,June Hyunkyung Lee,Sook-ja Son
http://dx.doi.org/10.17966/KJMM.2016.21.1.8 Epub 2016 April 07
Abstract
A case of cutaneous lesions on the left lower leg caused by Curvularia species in an 80-year-old immunocompetent woman is described in this report. The etiological agent was identified as Curvularia species based on its colonial and microscopic morphology in pure tissue culture. The lesions healed after a 9-week regimen of oral itraconazole and topical lanoconazole.
Keywords
Curvularia Itraconazole Phaeohyphomycosis
INTRODUCTION
Phaeohyphomycosis encompasses a clinical spectrum of heterogeneous diseases, which mainly includes cutaneous and subcutaneous damage, as well as some rare invasive infections. This disease is caused by pheoid or melanized fungi with melanin in cell walls and is characterized histopathologically by the presence of septate hyphae, pseudohyphae, and yeasts[1],[2],[3]. To date, the etiologic agents of phaeohyphomycosis include 60 genera and 109 species. The most common agents are Exophiala spp., Wangiella spp., and Phialophora spp[2],[4].
The genus Curvularia, a saprobic black mold, is composed of about 40 species[1]. Curvularia species were first described by Boedijn et al. in 1933[5]. Most of the species are pathogens of grains and plants; however, Curvularia infections in humans are relatively uncommon[1],[3],[6],[7]. In this report, we describe a case of cutaneous phaeohyphomycosis of the lower leg caused by Curvularia species infection.
CASE REPORT
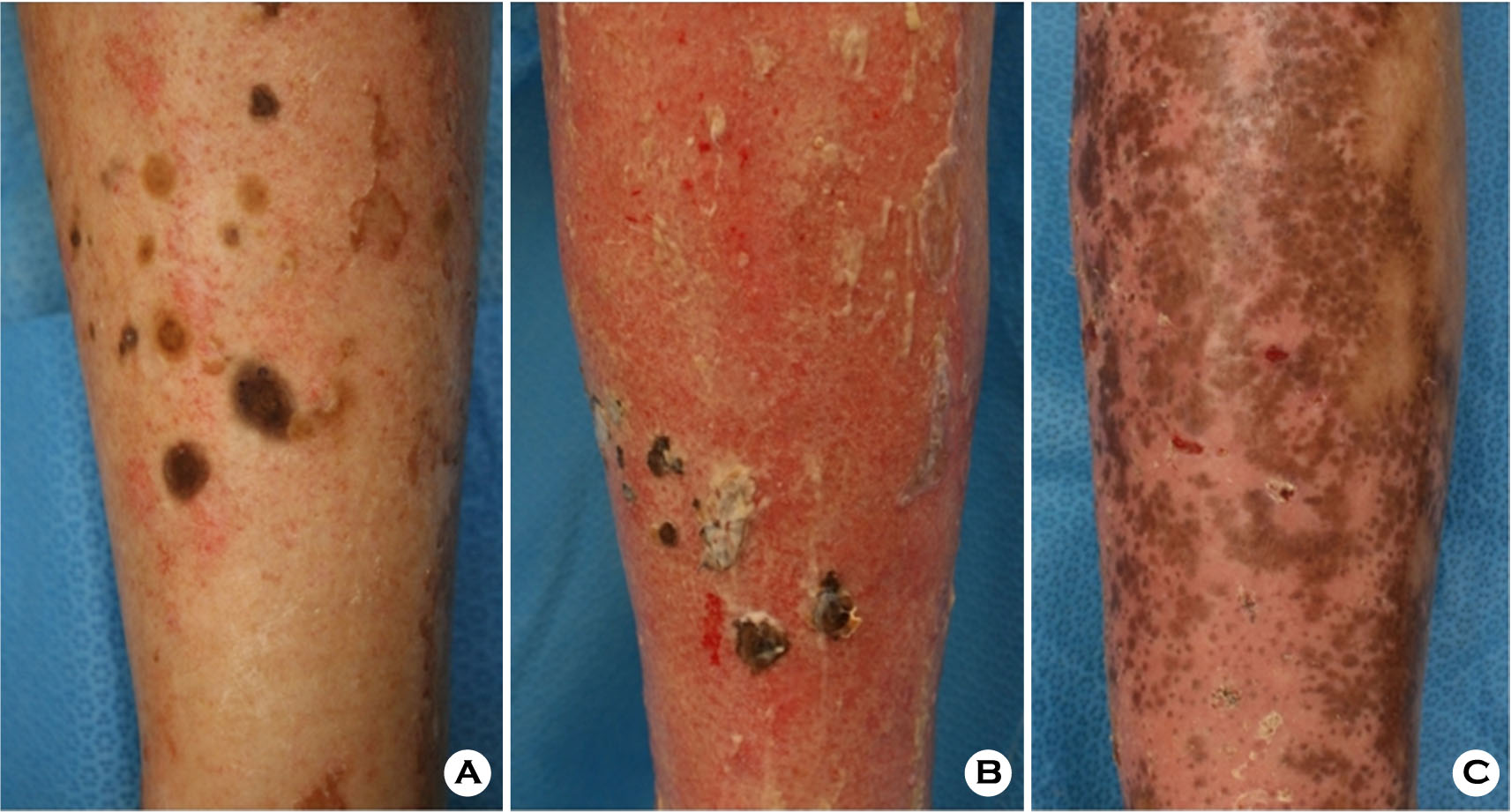
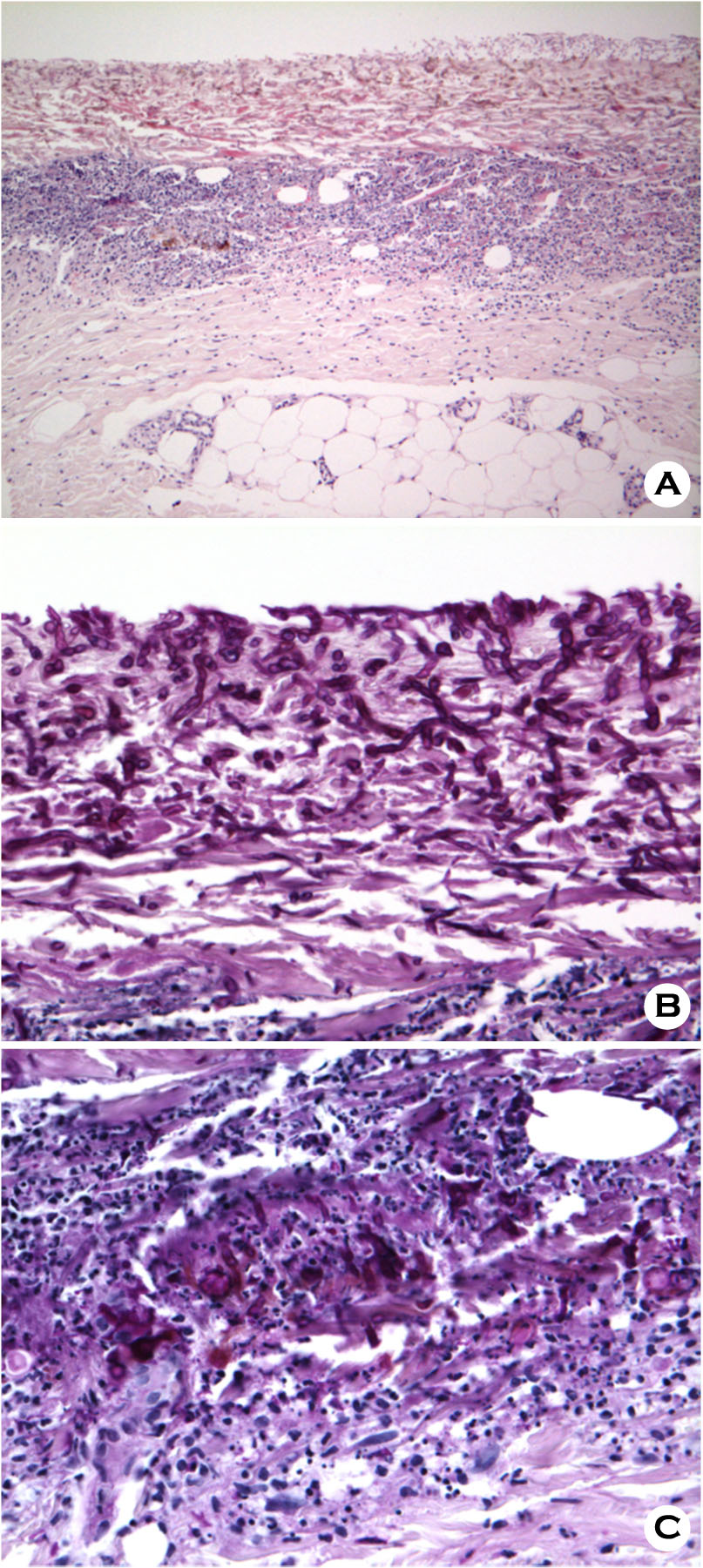
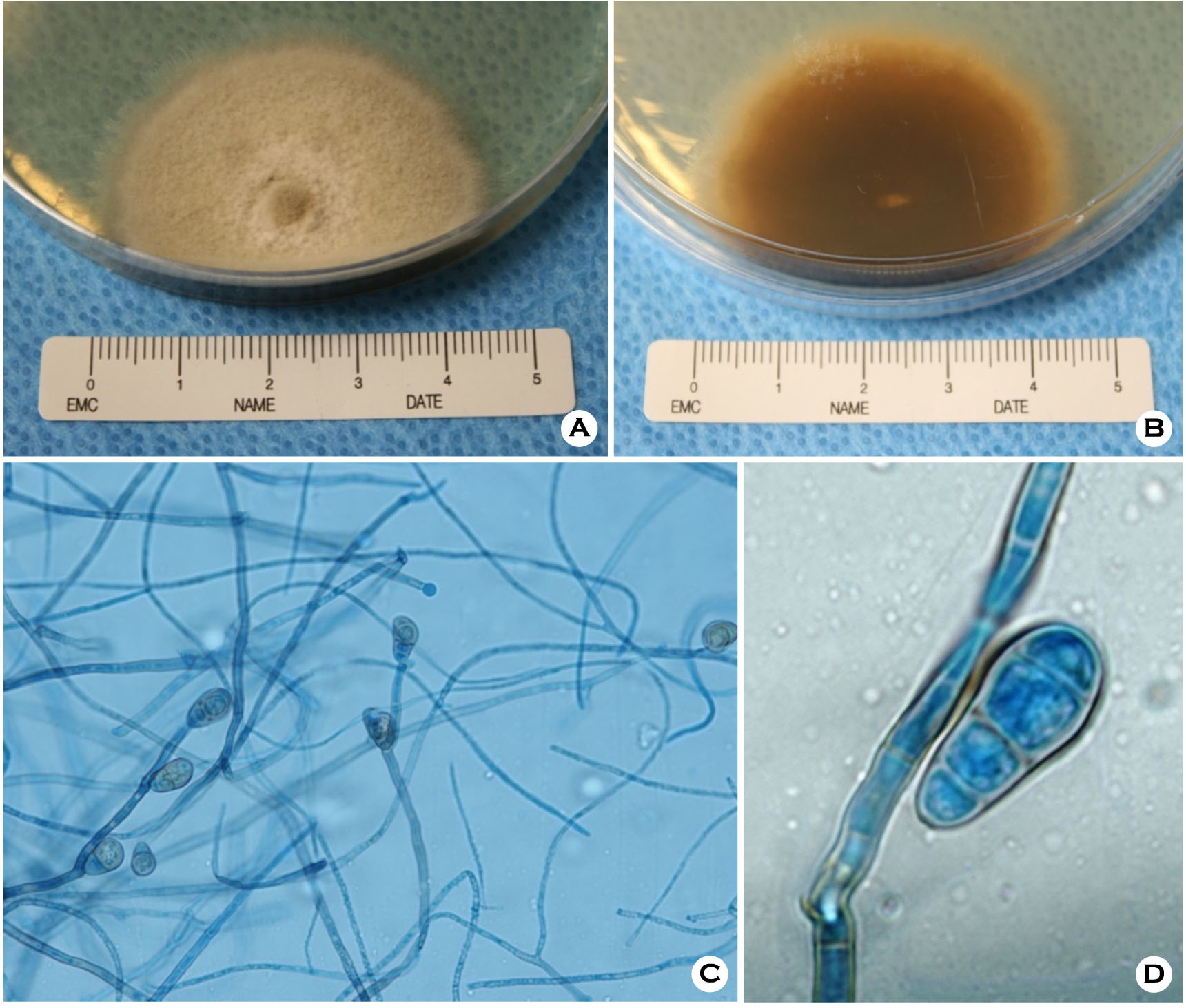
An 80-year-old Korean woman presented with a 1-month history of intensely pruritic dark brown patches on the left lower leg. She was healthy: neither immunocompromised nor suffering from diabetes mellitus, and was not on immunosuppressive medication. Examination revealed multiple, dark brownish colored, various sized, round patches with mild erosion on the left shin (Fig. 1A). Localized lymphadenopathy was absent, and she was afebrile. The results of laboratory studies revealed normal biochemical and immunological parameters. Her chest X-ray, chest CT, brain CT, ostiomeatal unit (OMU) CT showed no evidence of fungal infection. Lesional skin biopsies revealed brownish pigmented, irregular, septate hyphae and yeasts. Sparse, thick-walled, darkly pigmented, round, fungal cells and inflammatory cell infiltration were observed in the dermis by H&E and periodic acid-Schiff (PAS) staining, respectively (Fig. 2A-C). A part of the biopsied tissue was directly plated on to Sabouraud's dextrose agar and incubated at 25℃. The colony was downy, white to olive brown colored, and the diameter was 4.5 cm after 5 days, and the reverse side was flat and dark brown colored (Fig. 3A-B). Microscopic examination revealed curved poroconidia that had developed from a geniculate conidiophore. Conidiophores arose singly or in groups, terminal or lateral on septal hyphae, simple or branched, straight or flexuous, smooth-walled, pale to mid brown. Conidia were light brownish colored, curved, straight or pyriform, with multiple (3-to 4) transverse septae. The central cell of the conidia was darker and enlarged; therefore, 3-to 4-celled conidia appeared curved. Also, conidia were arranged singly or in groups in a sympodial manner at the tip or occasionally near the tip of the conidiophores, showing a typical geniculate growth pattern (Fig. 3C-D).
On the basis of these clinical, histopathological, and macro/microscopic morphological features, the isolate was identified as Curvularia species. The patient was started on oral itraconazole (400 mg/day) and topical lanoconazole. After 4 weeks, only a few skin patches and nodules persisted. Followup biopsy and culture were performed, and biopsy showed no fungal hyphae and no spores, and the culture showed no growth. The regimen was maintained for 9 weeks, and skin lesions subsided with post-inflammatory hyperpigmentation (Fig. 1B). Every 2 months, the patient comes to our outpatient clinic. And till now, during a year since she finished antifungal therapy she has shown no symptoms of local recurrence or visceral dissemination. And the skin lesions have completely disappeared.
DISCUSSION
Phaeohyphomycosis is a mycotic infection caused by a number of pheoid fungi whose morphologic characteristics in tissue include hyphae, yeast-like cells, or a combination of these[1],[2],[8]. Cases of phaeohyphomycosis due to pheoid fungi are increasing in frequency, especially in patients with severe immune dysfunction. A large diversity of genera of melanized fungi, such as Alternaria spp., Exophialaspp., and rarely Curvularia spp. are common causative pathogens of phaeohyphomycosis, while these fungi also exist ubiquitously in the environment[4],[6],[8].
Curvularia species have increasingly been reported to cause human diseases since it was first isolated from a mycetoma by Baylet et al. in 1959[6]. We have found only six reports of cutaneous phaeohyphomycosis due to Curvularia species without systemic infection in immunocompetent patients in the English literature (Table 1). Gugnani et al.[9] first reported a case of cutaneous phaeohyphomycosis in a 20-year-old female student with skin infection caused by C. clavata in 1990. The patient was treated with topical application of clotrimazole cream and the lesion cleared partially. Agrawal et al.[10] described two cases of cutaneous phaeohypho- mycosis caused by C. pallescens. Both patients were immunocompetent. Lesions were found on the feet, thigh and thumb and were irregularly marginated, pruritic black and occasionally purulent. C. pallescens were isolated in pure culture from the biopsy specimens, seperately. Oxiconazole was most effective in vitro against the pathogen. But the patients failed to return for the therapy after the laboratory investigations were complete. Hiromoto et al.[7] described a case of cutaneous phaeohyphomycosis in a 67-year-old man injured by falling tree. Curvularia species were isolated in pure culture from the biopsy specimen of the patient's left forearm. The patient received oral terbinafine treatment and the lesion subsided in a month. But 2 months later, the lesion regrew; hence, surgical resection was carried out, followed by oral itraconazole 100 mg/day for 4 months. In 2008, Fan et al.[3] reported a case of cutaneous phaeohyphomycosis in a 64-year-old male who worked as a farmer. Fungal elements were found in the exudate and biopsy specimen, and the isolate was identified as C. clavata. The skin lesions healed after a 12- week regimen of oral fluconazole (100 mg/day). Yanagihara et al.[11] described a case of cutaneous phaeohyphomycosis in a 74-year-old healthy man who had two tiny, pruritic, thick brown scales on the fourth interdigital web of the right foot. The brown fungus isolated from the scales was identified as Curvularia species, and treated with topical antifungal agents. Gunathilake et al.[12] also reported a case of mycetoma pedis caused by C. lunata infection. The patient was a farmer, and the lesion on the left ankle subsided with 12-month regimen of oral itraconazole (400 mg/day).
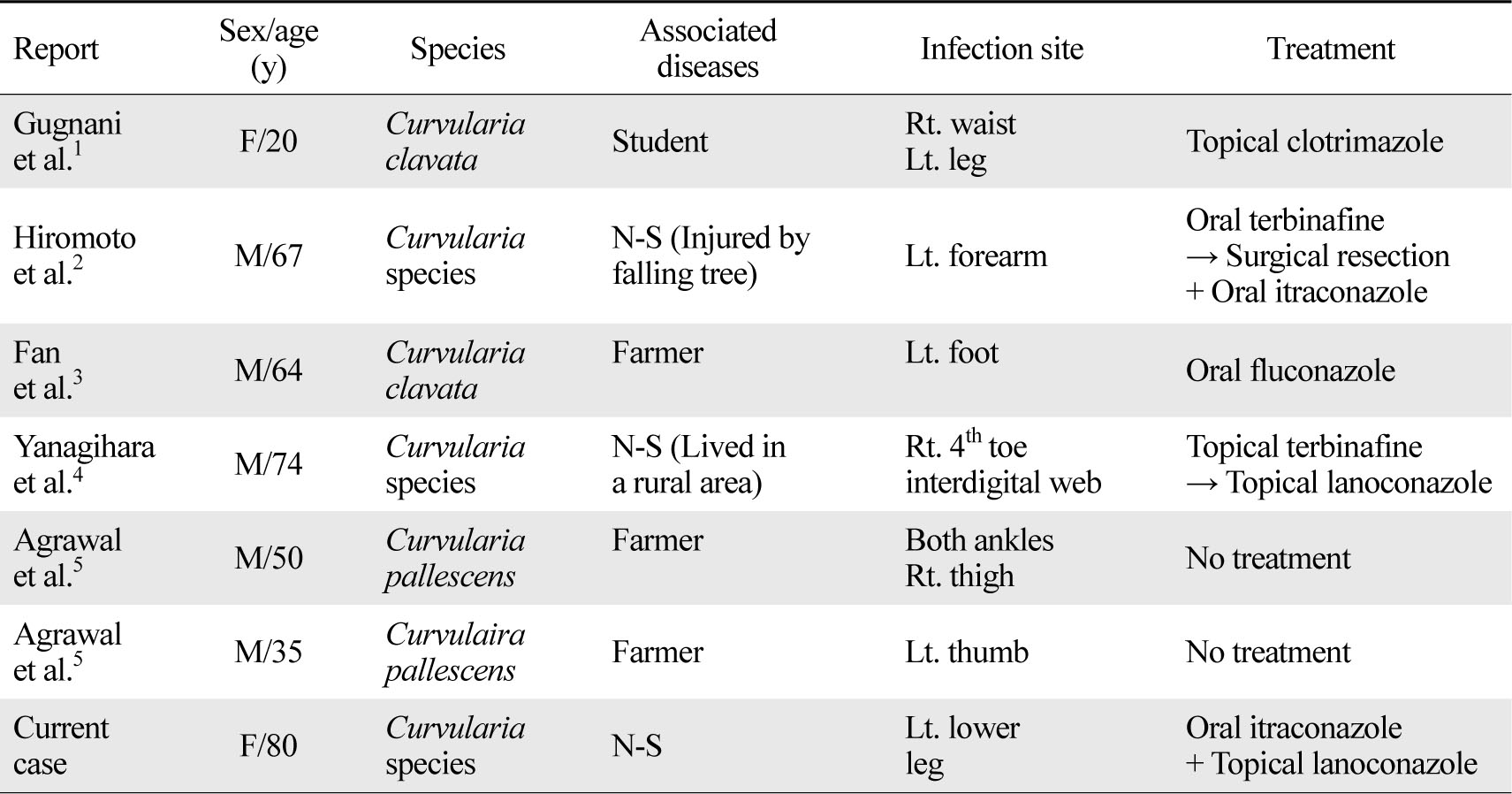
N-S: non-specific
The optimal antifungal therapy for cutaneous Curvularia infection is uncertain[1],[3],[4],[8]. Effective agents mainly include azoles and allylamines, and a daily dose of 400 mg oral itraconazole proved to be effective in many cases and is used as the most common regimen[1]. Treatment should be continued for several months or even longer, depending on to the patient's clinical condition. Oral terbinafine (250 mg/day), oral fluconazole (100 mg/day), oral posaconazole (20 mg/kg/day), oral voriconazole (25 mg/kg/day), and intravenous amphotericin B (0.25 mg/kg/day, up to 1 mg/kg) are also alternative antifungal chemotherapy regimens[1]. Topical antifungal cream application or additional surgical excision may be needed for better prognosis[11].
In the six cases mentioned above as well as in the present case, the patients were immunocompetent. Also, in all these six cases, the lesions occurred on exposed areas. Among the patients, three worked as farmers and one was injured by falling tree. Immunosuppression does not seem to be necessary for acquisition of Curvularia species infection[8]. Minor skin trauma might play an important role in the transmission, and therefore, avoiding scratch or injury is essential to prevent opportunistic mycoses[6],[8].
Herein, we report a unique and a rare case of cutaneous phaeohyphomycosis caused by Curvularia species in an immunocompetent woman. It is important for clinicians to be aware of the potential mycoses in trauma-prone sites in immunocompetent patients.
Conflict of interest
The authors declare no conflict of interest.
References
1. Fernandez M, Noyola DE, Rossmann SN, Edwards MS. Cutaneous phaeohyphomycosis caused by Curvularia lunata and a review of Curvularia infections in pediatrics. Pediatr Infect Dis J 1999;18:727 -731
Google Scholar
2. Revankar SG, Sutton DA. Melanized fungi in human disease. Clin Microbiol Rev 2010;23:884-928
Crossref
Google Scholar
3. Fan YM, Huang WM, Li SF, Wu GF, Li W, Chen RY. Cutaneous phaeohyphomycosis of foot caused by Curvularia clavata. Mycoses 2009;52:544-546
Crossref
Google Scholar
4. Isa-Isa R, García C, Isa M, Arenas R. Subcutaneous phaeohyphomycosis (mycotic cyst). Clin Dermatol 2012;30:425-431
Google Scholar
5. Manamgoda DS, Cai L, McKenzie EH, Crous PW, Madrid H, Chukeatirote E, et al. A phylogenetic and taxonomic re-evaluation of the Bipolaris-Cochliobolus -Curvularia complex. Fungal Diversity 2012;56:131 -144
Google Scholar
6. Carter E, Boudreaux C. Fatal cerebral phaeohyphomycosis due to Curvularia lunata in an immunocompetent patient. J Clin Microbiol 2004;42:5419 -5423
Crossref
Google Scholar
7. Hiromoto A, Nagano T, Nishigori C. Cutaneous infection caused by Curvularia species in an immunocompetent patient. Br J Dermatol 2008;158:1374 -1375
Crossref
Google Scholar
8. Guarro J, Gené J, Stchigel AM. Developments in fungal taxonomy. Clin Microbiol Rev 1999;12:454 -500
Google Scholar
9. Gugnani H, Okeke C, Sivanesan A. Curvularia clavata as an aetiological agent of human skin infection. Letters in Applied Microbiology 1990;10: 47-49
Crossref
Google Scholar
10. Agrawal A, Singh S. Two cases of cutaneous phaeohyphomycosis caused by Curvularia pallescens. Mycoses 1995;38:301-303
Crossref
Google Scholar
11. Yanagihara M, Kawasaki M, Ishizaki H, Anzawa K, Udagawa S-I, Mochizuki T, et al. Tiny keratotic brown lesions on the interdigital web between the toes of a healthy man caused by Curvularia species infection and a review of cutaneous Curvularia infections. Mycoscience 2010;51:224-233
Google Scholar
12. Gunathilake R, Perera P, Sirimanna G. Curvularia lunata: A rare cause of black-grain eumycetoma. J Mycol Med 2014;24:158-160
Crossref
Google Scholar