pISSN : 3058-423X eISSN: 3058-4302
Open Access, Peer-reviewed

pISSN : 3058-423X eISSN: 3058-4302
Open Access, Peer-reviewed
Kinanthi Koesandrini,Trisniartami Setyaningrum,Yuri Widia,Sylvia Anggraeni,Linda Astari,Evy Ervianti,Sunarso Soeyoso
10.17966/JMI.2025.30.4.149 Epub 2026 January 01
Abstract
Tinea capitis is a dermatophyte infection that affects the scalp hair follicles and is most commonly observed in children but uncommonly recognized during infancy. This study aimed to investigate a 2-month-old girl with a well-demarcated gray-patch alopecic plaque accompanied by fine scaling and broken, dull, and occasionally bent ("bamboo-like") hairs. Wood's lamp examination showed bright blue-green fluorescence along the infected hair shafts, while the trichoscopy findings showed comma and corkscrew hairs. A potassium hydroxide preparation confirmed an ectothrix pattern, and a fungal culture indicated the presence of Microsporum ferrugineum. The patient was orally administered griseofulvin with adjunctive topical ketoconazole, achieving a significant clinical improvement by Week 6. This case emphasizes the value of layered diagnostics (Wood's lamp examination, trichoscopy, KOH, and fungal culture) to establish an etiologic diagnosis in very young infants and to distinguish Microsporum—infections typically gray-patch with bright fluorescence—from other dermatophytes. Since topical agents do not reach the deep portion of hair follicles, systemic therapy is essential; griseofulvin remains the preferred first-line agent for treating ectothrix infections due to Microsporum. Household or pet exposure should be assessed to identify potential sources and prevent recurrence.
Keywords
Griseofulvin Microsporum ferrugineum Tinea capitis Trichoscopy Wood's lamp
Tinea capitis (TC) is a dermatophytosis of the scalp hair follicles caused by Microsporum and Trichophyton species. Microsporum typically invades the hair in an ectothrix pattern, in which the arthrospores are formed on the outer surface of the hair shaft, whereas Trichophyton usually presents as an endothrix infection with spores developing within the hair shaft. In Trichophyton schoenleinii infection, the pathogen initially invades the hair medulla and subsequently regresses, leaving air-filled tunnels within the hair shaft known as the favic pattern1,2.
TC is the most common fungal infection of the scalp in children aged 3-7 years and has also been increasingly re- cognized in infants2-4. Moreover, TC cases are rare in the first months of life. Its clinical manifestations are diverse, including alopecic patches, scaling, annular erythema, broken hairs, and—in inflammatory forms—kerion or favus. Delay in diagnosis and treatment may result in more extensive scalp involvement and complications such as permanent hair loss4.
The diagnosis of TC is supported by Wood's lamp exam- ination and trichoscopy/dermoscopy and confirmed by direct microscopy using potassium hydroxide (KOH) preparations of scalp scrapings and affected hairs, with subsequent fungal culture from the same specimens. The characteristic tricho- scopic patterns can also expedite a correct diagnosis1.
The first-line systemic therapies for TC include terbinafine, griseofulvin, itraconazole, and fluconazole, which are selected according to the likely or identified pathogen5. Clinically, gri- seofulvin remains the most effective agent for ectothrix Microsporum infections due to its fungistatic action that interferes with fungal microtubules, arresting mitosis and impairing cell wall synthesis. Such treatment is typically admin- istered for 6-8 weeks1-5. In the present study, we aimed to present a case of TC in a 2-month-old infant, emphasizing multimodal diagnosis and favorable response to griseofulvin.
This study investigated a 2-month-old Javanese girl who was referred to the Dermatology and Venereology outpatient clinic of Dr. Soetomo General Academic Hospital, Surabaya, with hair loss since birth, followed by progressive scalp redness over the preceding 4 weeks. Two weeks after birth, a hair clump with yellowish discharge was observed, which grad- ually enlarged and was followed by patchy hair loss and surrounding erythematous plaques. Pruritus and pain were not assessable. No history of preceding fever was noted. The patient's mother denied similar complaints among household contacts and any known fungal infections. The family had no pets, although many stray cats roamed around the house. Before referral, a pediatrician considered milk allergy and advised switching formula; however, no improvement was noted. A subsequent physician prescribed topical miconazole for 1 week, indicating no clinical response.
The patient showed no history of drug allergy or atopy. She was born at term via cesarean section (birth weight 2,800 g; length 48 cm). At presentation, she was developmentally appropriate and able to lift her head. Her weight was 4.5 kg and length 53 cm; the vital signs and general examination results were within normal limits.
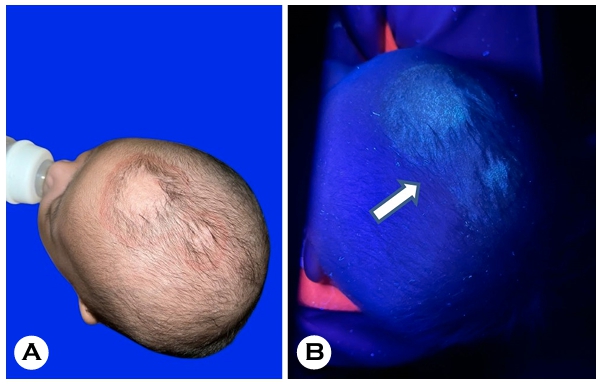
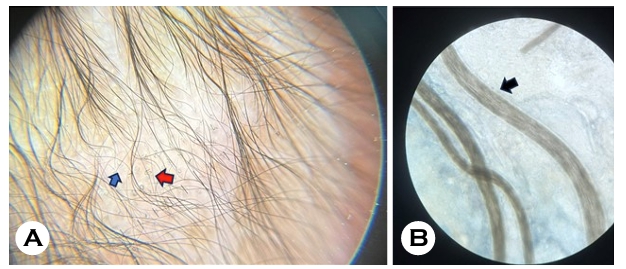
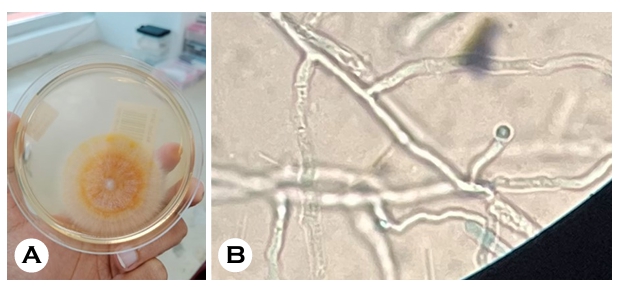
The dermatologic examination of the parietal scalp revealed alopecia with well-demarcated, gray-patch plaques measuring approximately 2 × 3 cm and 1 × 2 cm, with fine scaling and active borders. Many hairs within the plaques appeared dull and occasionally bent (bamboo-like) with broken hairs at the periphery (Fig. 1A). Wood's lamp examination in a dark room showed bright blue-green fluorescence along the infected hair shafts (Fig. 1B). The trichoscopy results showed comma hairs and corkscrew hairs on an erythematous, scaly back- ground (Fig. 2A; magnification ×20). The direct microscopy of the depilated hairs using 10% KOH revealed numerous ectothrix arthroconidia coating the hair shaft (Fig. 2B). The fungal culture of the hair fragments on SDA (incubated at a temperature of 25-28℃ for up to 4 weeks) yielded growth consistent with that of Microsporum ferrugineum, forming yellow, flat colonies with central folding and bundles of sub- merged hyphae at the periphery. The reverse showed bright yellow pigmentation (Fig. 3A). The microscopy of the culture showed long, straight hyphae with prominent cross-walls ("bamboo hyphae") and chlamydoconidia (Fig. 3B). Compared with M. audouinii, M. ferrugineum is usually more sparsely sporulating, with conidia absent or rare, and is characterized by "bamboo" hyphae and chlamydoconidia in culture. In contrast, Microsporum canis usually forms abundant large, thick-walled macroconidia with pointed ends and develops colonies with a characteristic yellow-green pigment.
A diagnosis of noninflammatory TC caused by Microsporum ferrugineum was made. The patient was treated with 62.5 mg of oral griseofulvin twice daily (a total of 125 mg/day; approxi- mately 28 mg/kg/day) and 2% of ketoconazole shampoo applied once daily to the scalp (contact time of ~3 minutes before rinsing). Follow-up was scheduled every 2 weeks. By Week 6, a significant clinical improvement was observed, with a reduction of scaling and erythema and visible regrowth of terminal hairs in previously alopecic areas (Fig. 4). No adverse events were noted.
The patient was diagnosed with noninflammatory type TC caused by Microsporum ferrugineum and was given com- bination antifungal treatment with griseofulvin (2 × 62.5 mg) and 2% ketoconazole shampoo applied on the scalp once daily for 3 minutes and then rinsed, with every 2 weeks of follow-up. Subsequently, the patient showed significant im- provement after 6 weeks of treatment, as indicated by hair growth in the previously bald area (Fig. 4).

Infantile TC is uncommon but should be suspected in young children presenting with alopecia, pruritus, and/or persistent desquamation with hair thinning; scalp lesions require myco- logic evaluation1-4. A previous review identified only ~50 reported TC cases in infants aged <1 year at the time of assessment, emphasizing its rarity2. Transmission to infants may occur through contact with asymptomatic carriers (children or adults), contaminated fomites (combs, towels, pillows, toys, brushes), or exposure to carrier pets1,2. In the present case, since the family lived in a rural setting with frequent ex- posure to stray cats, zoonotic or fomite transmission remained possible.
Although TC remains uncommon, recent literature suggests that it is increasingly recognized, with underreporting likely due to diagnostic delay and clinical overlap in early infancy. This suggests the value of layered diagnostics (Wood's lamp examination, trichoscopy, KOH, and fungal culture) in very young infants. Clinically, TC may range from subtle alopecia to well-demarcated, erythematous, scaly, nonscarring patches with broken hairs, often involving the occiput5. Our patient presented with symptoms of alopecia with annular erythema- tous plaques and active borders—features that are typical of TC. More specifically for Microsporum ferrugineum, classic des criptions emphasize a gray-patch pattern with dull, occa- sionally bent ("bamboo-like") hairs and broken hairs. Consist- ent with these characteristics, in the present case, several hairs within the plaques appeared dull and bent with peripheral broken hairs. Moreover, bright blue-green fluorescence based on Wood's lamp examination supported the Microsporum etiology. Wood's lamp fluorescence in Microsporum infection may vary in intensity depending on the stage of infection, previous topical treatments, environmental lighting, and device quality. Thus, faint fluorescence does not exclude M. ferrugineum, especially when supported by culture confirm- ation.
Overall, the clinical and trichoscopic findings were con- cordant with the classic profile of Microsporum ferrugineum, with minor variations likely reflecting the patient's very young age, disease stage, and brief prior topical exposure. Con- firmation by 10% KOH showing ectothrix spores and culture positive for M. ferrugineum supported the diagnosis and the selection of griseofulvin as first-line therapy.
The diagnostic work-up combined Wood's lamp examin- ation (green fluorescence), trichoscopy (characteristic comma and corkscrew hairs), and 10% KOH, demonstrating an ecto- thrix pattern—noninvasive tools that facilitate early recog- nition. Fungal culture remains essential for the identification of definitive species, particularly when systemic therapy is planned2-4. In the present case, fungal culture has identified Microsporum ferrugineum, while culture microscopy showed "bamboo hyphae," assisting differentiation from other Micro- sporum species.
The dermatophyte distribution varies geographically. At Dr. Soetomo General Academic Hospital, M. canis has been the most common species, followed by M. audouinii 4. Micro- sporum ferrugineum, an anthropophilic dermatophyte that induces ectothrix infection, can mimic M. audouinii or M. canis, necessitating careful distinction, while M. ferrugineum induces inflammatory erythematosquamous tinea corporis2. The differential diagnoses include seborrheic dermatitis, atopic dermatitis, neonatal lupus, and alopecia areata1-4. Atopic der- matitis was less likely given the absent personal/family history, while alopecia areata (typically nonscaling) was excluded by trichoscopic comma/corkscrew hairs.
In infants (<12 months), TC is relatively rare, and Micro- sporum ferrugineum has been reported as a nondominant cause among children aged <2 years based on recent epi- demiologic reviews. This emphasizes the value of culture and detailed mycologic characterization to confirm species, since treatment selection (e.g., griseofulvin for ectothrix infections caused by Microsporum) influences the clinical response and treatment duration. Griseofulvin remains the first-line therapy for ectothrix Microsporum infections (including M. canis, M. audouinii, and M. ferrugineum), generally for 6-8 weeks; alternatives include itraconazole or fluconazole1,2. Topical adjuvants may also help reduce surface fungal load (e.g., 1-2.5% selenium sulfide, 1-2% zinc pyrithione, 2.5% povidone-iodine, 2% ketoconazole) applied 2-4 times weekly for 2-4 weeks1,2. Our patient was administered oral griseofulvin 62.5 mg twice daily (~25 mg/kg/day) with 2% ketoconazole shampoo once daily. By Week 6, a significant improvement was observed: Wood's lamp examination showed no fluo- rescence, the trichoscopy results showed resolution of comma /corkscrew hairs, and KOH was negative. The administration of griseofulvin was continued for an additional 2 weeks to minimize recurrence risk, with evident hair regrowth by Week 6.
In summary, Wood's lamp examination and trichoscopy are valuable noninvasive modalities that facilitate early recognition and suggest likely species, while KOH and fungal culture confirm the diagnosis. Griseofulvin treatment remains the standard of care for ectothrix Microsporum infections and is widely used in pediatric practice.
Infantile tinea capitis is rare and often diagnostically chal- lenging. This case underscores the value of combining Wood's lamp, trichoscopy, KOH microscopy, and culture for accurate species identification. Prompt recognition of Microsporum ferrugineum and initiation of species-appropriate therapy with griseofulvin resulted in excellent clinical and mycologic resolution.
References
1. Petrucelli MF, Abreu MH, Cantelli BAM, Segura GG, Nishimura FG, Bitencourt TA, et al. Epidemiology and diagnostic perspectives of dermatophytoses. J Fungi 2020;6:310
Google Scholar
2. Gupta AK, Mays RR, Versteeg SG, Piraccini BM, Shear NH, Piguet V, et al. Tinea capitis in children: a systematic review of management. J Eur Acad Dermatol Venereol 2018;32:2264-2274
Google Scholar
3. Abtahi-Naeini B, Payandeh A, Rastegarnasab F. Successful treatment of fungal ball-associated tinea capitis in a healthy infant: An unusual presentation. Clin Case Rep 2023;11:e7752
Google Scholar
4. Elghblawi E. Tinea capitis in children: A report of four cases trichoscopic with trichoscopic features. Indian J Paediatr Dermatol 2018;19:51
Google Scholar
5. Aharaz A, Jemec GBE, Hay RJ, Saunte DML. Tinea capitis asymptomatic carriers: what is the evidence behind treatment? J Eur Acad Dermatol Venereol 2021;35: 2199-2207
Google Scholar
Congratulatory MessageClick here!