pISSN : 3058-423X eISSN: 3058-4302
Open Access, Peer-reviewed

pISSN : 3058-423X eISSN: 3058-4302
Open Access, Peer-reviewed
Presstisa Gifta Axelia,Trisiswati Indranarum,Linda Astari,Evy Ervianti
10.17966/JMI.2025.30.4.144 Epub 2026 January 01
Abstract
Primary cutaneous aspergillosis (PCA) is a rare form of Aspergillus infection that usually affects immunocompromised people. However, it also occurs in healthy individuals, where it is often mistaken for common dermatophyte infections. We describe a case of a 27-year-old woman, with a normal immune system, who developed persistent, itchy, red to darkened patches on both lower legs for over two years. Initial examination and KOH microscopy suggested tinea corporis. Despite using oral antifungal medications and topical urea cream, the lesions only improved slightly. A fungal culture later identified Aspergillus niger as the cause. She was treated with 200 mg of oral itraconazole daily and topical urea cream, resulting in significant improvement after eight weeks. PCA in patients with healthy immune systems is rare and often results from minor, unnoticed trauma introducing fungus. Although A. fumigatus and A. flavus are more common causes, A. niger is an uncommon culprit. This case highlights the diagnostic difficulties of PCA given its resemblance to a dermatophyte infection. Fungal culture is an important diagnostic step, if available. Healthcare providers should think about PCA in unusual or long-lasting skin conditions that do not respond to treatment, even in healthy individuals, to ensure quick diagnosis and proper antifungal therapy management.
Keywords
Aspergillosis Aspergillus niger Immunocompetent Itraconazole Tinea corporis
Primary cutaneous aspergillosis (PCA) is a rare condition, mainly affecting immunocompromised people, such as those with neutropenia, malignancies, or on immunosuppressive therapy. It usually develops when Aspergillus spp. is directly introduced into damaged skin, including areas with trauma, burns, surgical wounds, or occlusive dressings. However, recent reports have documented PCA in immunocompetent patients, where diagnosis is often delayed because of its nonspecific symptoms and resemblance to more common superficial fungal infections like tinea corporis. Oğuz et al. noted that out of 168 PCA cases reported across 114 articles from 1967 to 2017, the number of cases in immuno- competent patients was rather low1,2.
Among Aspergillus species, A. fumigatus and A. flavus are the most common pathogens involved in PCA, while A. niger is rarer. Since PCA is rare in immunocompetent indi- viduals and often resembles dermatophytosis, clinicians tend to rely heavily on clinical features and KOH microscopy, which may not always provide a definitive diagnosis. Cultures and, when available, histopathological examinations are crucial for confirmation. This case report describes an unusual instance of A. niger-caused PCA in an immunocompetent woman, initially mistaken for tinea corporis. The report emphasizes the diagnostic challenges and the need to consider other fungal infections in atypical and persistent dermatoses2.
A 27-year-old woman visited the dermatology outpatient department at Dr. Soetomo General Hospital with recurrent, itchy red patches on both lower limbs, lasting about two years. The lesions started on the right leg and gradually extended to the left. She described the rash as initially small, red patches she frequently scratched, causing excoriation and enlargement. Over time, the patches increased in number and size. Despite the chronicity, she denied systemic symptoms such as fever, malaise, cough, weight loss, or respiratory issues.
She previously saw a general practitioner a year ago and was empirically treated with oral ciprofloxacin and cetirizine without improvement. Later, a dermatologist prescribed oral antihistamines (mebhydroline 3 × 50 mg), oral corticosteroids (Dexamethasone 3 × 0.5 mg), oral griseofulvin (1 × 125 mg), and topical steroid cream, but the lesions persisted with minimal response over several months. Due to the refractory nature of the condition, she was referred to the tertiary care dermatology polyclinic for further assessment management.
The patient denied any prior trauma to the affected area, recent or past exposure to irritant chemicals, or use of over-the-counter topical medications. She has no significant medical history, including diabetes mellitus, hypertension, malig- nancy, or autoimmune conditions, and she also denies taking immunosuppressive drugs. Her social history indicates she previously worked as a pharmacist and is now unemployed. Residing in a rural area near agricultural fields, she may have been exposed to fungal spores in the general environment. There is no family history of similar skin issues or other chronic dermatologic conditions.
Dermatologic examination showed multiple patches on both cruris, mainly on the front and lateral sides of the right and left lower legs (Fig. 1). The lesions were erythematous to hyperpigmented, with clearly defined borders, covered with fine scales, and had slightly raised active edges. There were no pustules, ulceration, or signs of secondary bacterial infection noted.

Initial examination of skin scrapings with 20% potassium hydroxide (KOH) revealed thin septate hyphae, initially in- dicating tinea corporis (Fig. 2). To confirm the diagnosis, a fungal culture was conducted. The patient was prescribed oral griseofulvin 250 mg twice daily and urea 10% cream twice daily. She was also advised to refrain from manipulating the lesions and to return to the polyclinic for evaluation in two weeks.

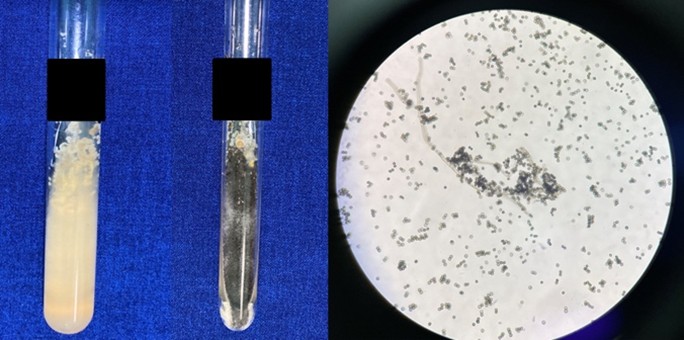
At the 14-day follow-up, the patient reported slight impro- vement in the lesions, with some fading of erythema and a change to hyperpigmented patches. However, pruritus and scales persisted, especially with heat and sweating. Derma- tological findings remained largely unchanged, showing persistent annular patches with scales. KOH exam revealed thin, septate hyphae. The fungal culture produced colonies that first appeared white, then turned black, with a white periphery and a cottony to granular texture, and a pale reverse surface. The culture was grown on Sabouraud dextrose agar and incubated for 14 days. Microscopic analysis at 40× magnification showed thin, septate hyphae with globose black conidia, consistent with Aspergillus niger (Fig. 3). PCR testing was not available at the hospital. A punch skin biopsy was not performed.
A final diagnosis of PCA was established based on clinical appearance and culture results. The patient started on oral itraconazole 200 mg daily and continued topical 10% urea cream. She was advised to strictly avoid using any topical corticosteroids or unprescribed medications.
Follow-up at week 4 showed partial lesion resolution, with decreased erythema, patches, scales, and itching. KOH exam- ination was negative for fungi at this point (Fig. 4). By week 8, there was notable clinical improvement, including the resolution of active edges, fewer patches and scales, hyper- pigmentation, and no new lesions. The patient tolerated itraconazole well, without adverse effects. She continued to be monitored clinically, with no evidence of systemic spread or recurrence observed up to seven months later.

PCA is a rare but clinically significant skin infection caused by direct inoculation of Aspergillus spp. into damaged skin. It primarily affects immunocompromised individuals; however, increasing evidence indicates that immunocompetent people are also at risk, especially in settings with high exposure and minor skin barrier disruptions. This case emphasizes a common yet often overlooked clinical scenario: PCA in an immuno-competent patient with chronic lesions that mimic superficial dermatophytosis. Healthcare providers should consider other fungal infections, particularly when the presentation is atypical or the condition persists despite treatment dermatoses.
Diagnosing cutaneous aspergillosis can be challenging be- cause the lesions often resemble tinea corporis, with KOH tests revealing septate hyphae. However, these lesions typic- ally do not respond to standard antifungal treatments. This reveals a key diagnostic limitation: although KOH microscopy is sensitive for detecting fungal elements, it cannot specify the fungal species. Fungal cultures are needed to identify the causative organism and determine appropriate treatment, but they take several days for growth and species identi- fication. This delay complicates treatment, especially with non-dermatophyte molds like Aspergillus. This diagnostic difficulty highlights the need to consider other mycoses, particularly in cases of chronic, treatment-resistant lesions, even in immuno- competent individuals.
The pathogen identified here, A. niger, is an uncommon but increasingly recognized cause of skin infections. Usually dismissed as a contaminant unless clinical signs strongly indicate infection, its consistent morphology and lack of other causes suggest it was truly pathogenic in this case. This report adds to the limited evidence of A. niger causing PCA in immune-competent individuals, emphasizing the growing number of cutaneous aspergillosis cases3. When evaluating differential diagnoses based on fungal results, Aspergillus species are primary considerations. While A. niger was iden- tified through its characteristic black colonies and globose conidia, other species such as A. fumigatus and A. flavus are also relevant. A. fumigatus generally forms grey-black colonies, and A. flavus produces yellow-green colonies—both distin- guishable from the black pigmentation observed here here4,5.
Clinically, PCA can present in various forms; the primary lesion may evolve from a macule or papule to a nodule or granulated tissue. It can also originate from superficial, spreading macerated or ulcerative lesions, influenced by host factors and fungal virulence. In this case, the erythematous patches with fine scales and active borders resembled der- matophyte infections. Although dermoscopy is a useful tool in evaluating superficial fungal infections, its diagnostic specificity for PCA is limited because there are few established criteria6.
Fungal culture remains the gold standard for identifying species. While it is often underused in resource-limited or busy clinical settings, it is essential for atypical, chronic, or treatment-resistant lesions. Once PCA is confirmed, prompt treatment is critical. Treatment options include systemic ther- apies such as polyenes like amphotericin B and its liposomal form, azole antifungals like voriconazole, posaconazole, and itraconazole, as well as echinocandins such as caspofungin and micafungin5. Surgical debridement is also advised as an additional antifungal treatment for severe cases to improve success rates. In this instance, a culture confirmed the presence of A. niger, allowing for the initiation of suitable systemic antifungal therapy. The patient responded positively to oral itraconazole, a triazole antifungal known to be effective against Aspergillus spp4,7-8, highlighting the importance of species-specific therapy in managing fungal skin infections. The patient received oral itraconazole 200 mg/day for 8 weeks with favorable clinical outcome and KOH evaluation. Other case reports also showed good efficacy of oral itraconazole 200 mg/day for 12-13 weeks9. A first-line treatment of PCA has not been established, with the duration of treatment varying depending on the disease severity and immunity status9.
This case contributes significantly to the clinical literature by illustrating that PCA—especially caused by A. niger—can mimic tinea corporis and persist despite standard antifungal treatments. The implications are substantial: clinicians should perform fungal culture in cases of atypical or recalcitrant superficial dermatoses, even in the absence of classical risk factors. Moreover, increased awareness of PCA's diverse presentations in immunocompetent individuals may lead to earlier intervention, reduce morbidity, and prevent progression to systemic disease1.
In a broader sense, this report promotes a more detailed diagnostic approach to unusual or chronic dermatologic infections. It questions the idea that being immunocompetent automatically means protection from invasive or atypical mycoses and highlights the ecological fact that fungal pathogens—widespread in soil, air, and organic material—can take any chance to invade. This emphasizes the importance of dermatologists staying alert in diagnosis and using culture tests to confirm when the clinical situation diverges from the norm.
This case highlights the vital need to consider PCA as a possibility, even in immunocompetent patients exhibiting unusual or persistent, treatment-resistant skin conditions. Its resemblance to common superficial fungal infections like tinea corporis complicates diagnosis and treatment. Reporting a rare case of PCA caused by A. niger in an immunocompetent individual, this document enhances the limited knowledge on atypical cases and emphasizes the importance of fungal culture for accurate diagnosis. It underscores the need for clinicians to expand their differential diagnosis and provides valuable insights for earlier detection and proper management of PCA, aiming to reduce morbidity and improve outcomes.
References
1. Avkan-Oğuz V, Çelik M, Satoglu IS, Ergon MC, Açan AE. Primary cutaneous aspergillosis in immunocompetent adults: three cases and a review of the literature. Cureus 2020;12:e6600
2. Tahir C, Garbati M, Nggada HA, Yawe EH, Abubakar AM. Primary cutaneous aspergillosis in an immunocompetent patient. J Surg Tech Case Rep 2011;3:94-96
Google Scholar
3. Merad Y, Derrar H, Belmokhtar Z, Belkacemi M. Aspergillus genus and its various human superficial and cutaneous features. Pathogens 2021;10:1-17
Google Scholar
4. Sheilaadji MU, Agusni I, Astari L, Anggraeni S, Widia Y, Ervianti E. Cutaneous aspergilosis caused by Aspergillus flavus: A case report. Berk Ilmu Kesehat Kulit dan Kelamin 2021;33:72-77
Google Scholar
5. Zhang R, Zhang Y, Xu W, Han X, Zhao J. Primary cutaneous aspergillosis due to Aspergillus fumigatus in an immunocompetent patient with diabetes mellitus after tattooing: A case report and review of literature. Infect Drug Resist 2023;16:791-797
Google Scholar
6. Tatara AM, Mikos AG, Kontoyiannis DP. Factors affecting patient outcome in primary cutaneous aspergillosis. Medicine (Baltimore) 2016;95:e3747
Google Scholar
7. Nacea DI, Enescu DM, Tatar R, Orzan OA, Diaconu LS. New challenges in the diagnosis and treatment of primary cutaneous aspergillosis in extensive pediatric burns. J Fungi 2025;11:281
Google Scholar
8. Park KD. Diagnosis and treatment of cutaneous asper- gillosis. J Mycol Infect 2021;26:83-86
Google Scholar
9. Nakashima K, Yamada N, Yoshida Y, Yamamoto O. Primary cutaneous aspergillosis. Acta Derm Venereol 2010;90:519-520
Google Scholar
Congratulatory MessageClick here!