pISSN : 3058-423X eISSN: 3058-4302
Open Access, Peer-reviewed

pISSN : 3058-423X eISSN: 3058-4302
Open Access, Peer-reviewed
Ramya Krishnan,Aswini Munirathinam,Priyadarshini Shanmugam
10.17966/JMI.2025.30.4.140 Epub 2026 January 01
Abstract
The co-occurrence of tuberculous mastitis and infiltrating ductal carcinoma of the breast is a rare clinical phenomenon that poses significant diagnostic and therapeutic challenges. Breast tissue is relatively resistant to tubercular infection, rendering breast tuberculosis an uncommon extrapulmonary manifestation. The overlapping clinical and radiological features of both diseases complicate the diagnostic process. This report presents the case of a 38-year-old woman diagnosed with both conditions concurrently. The diagnosis was established based on histopathological examination and microbiological confirmation, including the GeneXpert Mycobacterium tuberculosis (MTB) assay/resistance to rifampicin (RIF) assay, which detected MTB with an indeterminate rifampin resistance. Despite the indeterminate result, rifampin was included in the treatment regimen, in accordance with national guidelines and clinical judgment in the absence of confirmed resistance. This case is remarkable for its infrequency and highlights the importance of sensitive clinical suspicion, comprehensive evaluation, and coexistent pathologies in endemic regions. A comparison with existing literature highlights its novelty and clinical implications.
Keywords
Breast carcinoma Breast tuberculosis Caseous necrosis Dual pathology GeneXpert Histopathology Infiltrating ductal carcinoma
Tuberculosis (TB), caused by Mycobacterium tuberculosis (MTB), primarily affects the lungs but can also involve extra- pulmonary sites. Among these, breast TB is particularly rare, accounting for <0.1% of all breast pathologies. Its low incidence is attributed to the inherent resistance of breast tissue to MTB, possibly owing to limited lymphatic drainage and the high oxygen tension, which is unfavorable to bacilli growth.
Globally, TB remains a major public health concern, with approximately 10 million cases and 1.5 million deaths annually, despite being preventable and curable1. Concurrently, breast carcinoma is the most frequently diagnosed cancer among women, with approximately 2.3 million new cases annually2. Although both conditions are individually prevalent, the co- existence of breast TB and carcinoma in the same patient is exceedingly rare and often underdiagnosed because of overlapping presentations and imaging findings.
This report presents a rare case of tuberculous mastitis coexisting with infiltrating ductal carcinoma in a young woman. It highlights the diagnostic challenges, immunopathogenesis, and therapeutic implications. Additionally, this case adds to the limited existing literature on such concurrent pathologies and offers a critical comparison with previously reported cases to underscore its clinical novelty.
A 38-year-old woman, with no known comorbidities or previous TB exposure, presented with swelling in the left axilla for 6 months and a palpable lump in the left breast for 3 months. The breast lump was associated with intermittent pain over the past month, with no history of nipple discharge, weight loss, fever, or trauma. Vitals were stable, and systemic examination was unremarkable. On local examination, both breasts were symmetrical without any skin changes, such as ulceration, dimpling, or peau d'orange appearance. The nipples appeared normal. A 4 × 3 cm firm, mobile lump was palpated in the upper outer quadrant (4-5 o'clock position) of the left breast. Additionally, a 3 × 2 cm palpable lymph node was noted in the left axilla. The right breast and axilla were unremarkable. The differential diagnosis included both malignancy and TB. The Mantoux test was positive, showing 15-mm induration. A core-needle biopsy of the breast lesion was performed and submitted for histopathological evalu- ation and microbiological testing, including Ziehl-Neelsen (ZN) staining and the GeneXpert MTB/resistance to rifampicin (RIF) assay. The results of these investigations are presented in Fig. 1. MRI revealed two well-defined lesions in the lower and outer quadrants of the left breast, measuring 2.6 × 2.0 and 3.0 × 2.0 cm, respectively. Both lesions appeared hypointense on T1-weighted images and hyperintense on T2-weighted images, with rim enhancement suggestive of necrotic or infective components. Additionally, a significantly enlarged left axillary lymph node measuring 7.3 × 3.8 cm was noted. These findings were categorized as per the Breast Imaging Reporting and Data System (BI-RADS) VI and are shown in Figs. 2 and 3. Histopathological examination revealed features consistent with infiltrating ductal carcinoma. Granulomatous inflammation with caseous necrosis was noted in adjacent areas (Fig. 4). ZN staining of the biopsy specimen identified acid-fast bacilli. The GeneXpert MTB/RIF assay detected MTB DNA with an indeterminate result for rifampin resistance. Despite this, rifampin was included in the initial treatment regimen based on clinical judgment and in accordance with national TB control guidelines while awaiting further sus- ceptibility results. The patient underwent a modified radical mastectomy. Postoperatively, anti-tuberculous therapy was initiated using the standard 6-month regimen, consisting of isoniazid, rifampin, pyrazinamide, and ethambutol for the initial 2 months, followed by isoniazid and rifampin for remaining 4 months. Vitamin B6 supplementation was also initiated. The oncologic treatment was tailored based on the tumor stage and histological grading. The patient is currently under regular follow-up, with no evidence of disease recur- rence or TB reactivation.
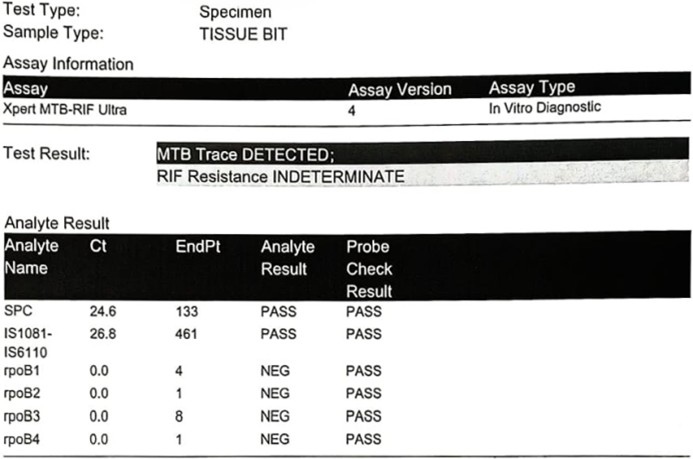
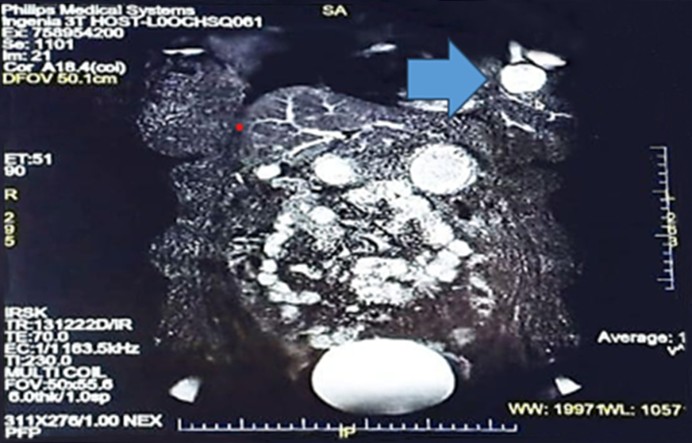

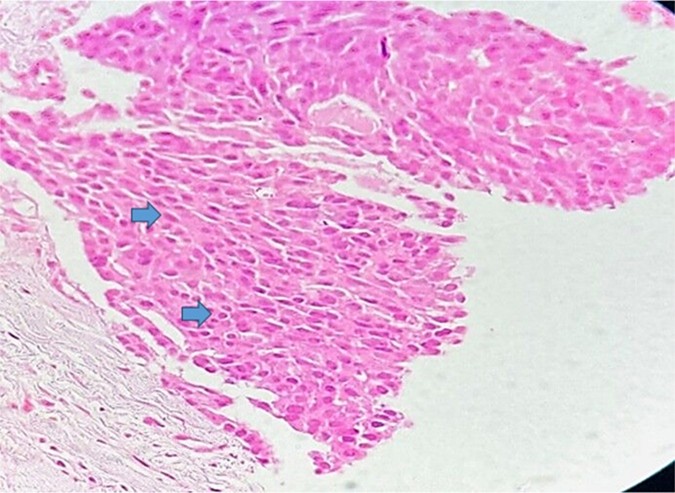
The coexistence of tuberculous mastitis and infiltrating ductal carcinoma of the breast represents a rare and diag- nostically challenging clinical case. This rarity is due in part to the relative resistance of the breast tissue to MTB infection. This phenomenon is attributed to factors such as limited lymphatic supply, sparse reticuloendothelial tissue, and high oxygen content, which are unfavorable for mycobacterial proliferation. Consequently, breast TB accounts for <0.1% of all breast lesions, even in TB-endemic regions3,4. The simul- taneous presence of TB and malignancy in the breast can lead to significant diagnostic confusion. Both conditions can exhibit similar clinical features, including palpable mass, axillary lymphadenopathy, and skin changes. Radiologically, both TB and carcinoma can appear as irregular, speculated masses on mammography or as hypoechoic lesions on ultrasonography. MRI findings are often inconclusive because both lesions may exhibit rim enhancement and hyperintensity on T2-weighted images. In the present case, the MRI findings indicated a BI-RADS VI lesion, necessitating further histopathological evaluation5. Histologically, TB is characterized by granuloma- tous inflamation with caseous necrosis and the presence of Langhans giant cells, whereas carcinoma is identified by malignant epithelial cells with nuclear atypia and stromal in- vasion. In the present case, both histopathological patterns were evident. This concurrent pathology was further con- firmed by ZN staining and the GeneXpert MTB/RIF assay, which detected MTB DNA. The GeneXpert result indicated an indeterminate status of rifampin resistance. Despite this, rifampin was incorporated in the anti-TB regimen based on World Health Organization guidelines and national TB proto- cols, which recommend initiating first-line treatment while waiting for the results of further susceptibility testing unless resistance is confirmed. This clinical decision was justified by the absence of risk factors for multidrug-resistant TB and the patient's good clinical response to the standard regimen6. The immunological interplay between chronic TB and carcino- genesis is still being investigated. Some studies have sug- gested that chronic inflammation and cytokine release in TB may contribute to DNA damage and malignant transform- ation. Conversely, malignancy-induced immune suppression may reactivate latent TB. However, the precise mechanisms remain speculative and are not yet fully understood7. Several studies have documented either sequential or simultaneous occurrence of breast carcinoma and TB8-10; however, most studies are limited to older age groups or isolated case series. The presented case differs in that it presents in a relatively younger woman (aged 38 years) with no significant comor- bidities or immunosuppression. Unlike most published reports, the present report highlights the use of molecular diagnostic tools (GeneXpert), which aided in the rapid identification of TB. Although Pandya J reported moderate sensitivity (83.3%) and high specificity (99%) for GeneXpert in tuberculous mastitis11, few case reports have discussed its utility in cases of coexisting carcinoma and TB12,13. This underscores the originality and clinical novelty of this report. The coexistence of both TB and carcinoma requires an individualized thera- peutic approach. In the presented case, the patient under- went surgical excision for carcinoma, followed by a standard anti-TB regimen. This approach ensured that neither disease was undertreated. Importantly, oncologic treatments such as chemotherapy may exacerbate or reactivate latent TB, reinforcing the need for thorough screening and concurrent TB management in endemic regions.
This case highlights the rare but clinically significant co- existence of tuberculous mastitis and breast carcinoma. Given the overlapping clinical and radiological features, a high index of suspicion and thorough diagnostic evaluation, including histopathology, microbiology, and molecular testing, are essential for accurate diagnosis. The case validates the value of GeneXpert in confirming TB even in complex oncologic settings, despite indeterminate resistance patterns. This report adds to the limited literature on this dual pathology and emphasizes the importance of increased clinical awareness, particularly in TB-endemic regions. Comprehensive manage- ment addressing both conditions is critical to optimizing patient outcomes. More studies exploring the immunological interactions between chronic TB and malignancy may provide deeper insights into this uncommon but important clinical entity.
References
1. Villar-Hernández R, Ghodousi A, Konstantynovska O, Duarte R, Lange C, Raviglione M. Tuberculosis: Current challenges and beyond. Breathe (Sheff) 2023;19:220166
2. Arnold M, Morgan E, Rumgay H, Mafra A, Singh D, Laversanne M, et al. Current and future burden of breast cancer: Global statistics for 2020 and 2040. Breast 2022; 66:15-23
Google Scholar
3. Murfee WL, Breslin JW. Linking lymphatic function to disease. J Physiol 2020;598:3065-3066
Google Scholar
4. Tulasi NR, Raju PC, Damodaran V, Radhika TS. A spectrum of coexistent tuberculosis and carcinoma in the breast and axillary lymph nodes: Report of five cases. Breast 2006;15:437-439
Google Scholar
5. Heidary M, Shirani M, Moradi M, Goudarzi M, Pouriran R, Rezaeian T, et al. Tuberculosis challenges: Resistance, co-infection, diagnosis, and treatment. Eur J Microbiol Immunol (Bp) 2022;12:1-17
Google Scholar
6. Singh AK, Gupta P, Verma N, Khare V, Ahamad A, Verma V, et al. Fungal rhinosinusitis: Microbiological and histopathological perspective. J Clin Diagn Res 2017;11: DC10-DC12
Google Scholar
7. Yan W, Zheng Y, Dou C, Zhang G, Arnaout T, Cheng W. The pathogenic mechanism of Mycobacterium tuber- culosis: implication for new drug development. Mol Biomed 2022;3:48
Google Scholar
8. Miller RE, Salomon PF, West JP. The coexistence of carcinoma and tuberculosis of the breast and axillary lymph nodes. Am J Surg 1971;121:338-340
Google Scholar
9. Hovanessian Larsen LJ, Peyvandi B, Klipfel N, Grant E, Iyengar G. Granulomatous lobular mastitis: Imaging, diagnosis, and treatment. American J Roentgenol 2009; 193:574-581
Google Scholar
10. Al-Khawari HA, Al-Manfouhi HA, Madda JP, Kovacs A, Sheikh M, Roberts O. Radiologic features of granuloma- tous mastitis. Breast J 2011;17:645-650
Google Scholar
11. Pandya J, Tiwari AR, Thareja V. Role of gene Xpert MTB /RIF assay for diagnosis of tuberculous mastitis. Indian J Surgery 2021;83:341-344
Google Scholar
12. Bani-Hani KE, Yaghan RJ, Matalka II, Mazahreh TS. Tuberculous mastitis: a disease not to be forgotten. Int J Tuberc Lung Dis 2005;9:920-925
Google Scholar
13. Alzaraa A, Dalal N. Coexistence of carcinoma and tuber- culosis in one breast. World J Surg Oncol 2008;6:29
Google Scholar
Congratulatory MessageClick here!