pISSN : 3058-423X eISSN: 3058-4302
Open Access, Peer-reviewed

pISSN : 3058-423X eISSN: 3058-4302
Open Access, Peer-reviewed
Jonghae Kim
10.17966/JMI.2025.30.2.37 Epub 2025 July 01
Abstract
Deep neck infections pose significant challenges for airway management due to swelling of soft tissues, formation of abscesses, and limited jaw and neck movement, which increase the risk of serious airway obstruction. Administering general anesthesia in such cases can worsen airway obstruction, making awake intubation the method of choice. Using fiberoptic bronchoscopy for awake nasotracheal intubation provides airway security while allowing spontaneous breathing, thus minimizing the risk of total airway blockage. This review covers the pathophysiology of airway compromise associated with deep neck infections, the indications and contraindications for awake intubation, and the vital techniques for executing fiberoptic bronchoscopy-guided awake nasotracheal intubation. Key procedural steps include careful patient monitoring, oxygenation, premedication, topical anesthesia, and sedation to ensure a successful procedure. Technically, a tracheal tube is maneuvered into the tracheal lumen over the fiberoptic bronchoscope's insertion cord, which is previously placed within the trachea. When done correctly, this approach enhances patient safety by avoiding airway collapse and ensuring controlled airway access during the induction of general anesthesia. Fiberoptic bronchoscopy-guided awake intubation remains essential in managing difficult airways in patients with deep neck infections undergoing general anesthesia.
Keywords
Airway management Bronchoscopes General anesthesia Infection Intubation
Deep neck infections (DNIs) are severe infections that affect the potential spaces formed by the mucous membranes lining the pharyngeal cavity and the layers of the deep cervical fascia1,2, typically arising from dental infections, tonsillitis, pharyngeal trauma, or foreign body impaction. This infection can disseminate quickly, resulting in sepsis, necrotizing fasciitis, or mediastinitis3,4. Antibiotics typically manage this condition; however, surgical drainage is necessary if the treatment is ineffective or the abscesses are large. Since soft tissue swell- ing or abscess formation can distort airway anatomy and restrict jaw and neck movement, airway management for DNI patients becomes challenging5. Using general anesthesia for surgical drainage can obstruct the airway, making airway management more complicated6. Total airway obstruction hampers manual ventilation and worsens existing hypoxia, necessitating immediate actions like tracheal intubation, placement of a supraglottic airway, or performing a trache- otomy. However, altered airway anatomy and restricted jaw and neck movement complicate intubation via laryngoscopy and hinder supraglottic airways from achieving a proper anatomical seal around the pharyngolaryngeal structures5. Unidentifiable surface landmarks due to the distorted airway anatomy also complicate tracheotomy. To address clinical issues linked to general anesthesia in DNI patients, awake intubation is advised7 because it maintains spontaneous respiration while securing the airway. This narrative review explores the technical aspects of fiberoptic bronchoscopy-guided awake nasotracheal intubation (FBAI). It highlights that tracheal tube insertion through the nasal route is well tolerated, provides a more straightforward bronchoscopic approach, and is suitable for patients with limited mouth opening, a large tongue, or a fixed flexed neck. Additionally, it addresses the pathophysiology of DNI-induced airway compromise and the indications and contraindications for this procedure (FBAI).
PATHOPHYSIOLOGY OF AIRWAY COMPROMISE
DNIs may affect the parapharyngeal, retropharyngeal, sub- mandibular, or prevertebral spaces. If they progress or involve multiple spaces, they can lead to soft tissue edema, abscess formation, restricted neck motion, or trismus, which may com- promise the airway8. The retropharyngeal and parapharyngeal spaces are particularly concerning because they are near the airway and can quickly lead to mediastinitis. In cases of Ludwig's angina that arise from submandibular space infec- tions, the swelling in the submandibular space displaces the tongue upward and backward, causing progressive airway obstruction9,10. Edema, inflammation, and abscess formation can significantly reduce the airway lumen, eventually leading to complete obstruction of the airway11. Trismus caused by infections in the masticator space complicates direct laryngos- copy, thus making airway management more challenging. Therefore, prompt assessment and intervention are vital to avert life-threatening airway issues.
INDICATIONS AND CONTRAINDICATIONS FOR AWAKE INTUBATION
Since its first use in 196712, FBAI has been a mainstay of the management of predicted difficult airway13. Awake intubation is necessary for patients facing imminent airway obstruction while being able to sustain their airway and breathe spon- taneously. This approach is particularly beneficial in cases where difficult tracheal intubation and face mask ventilation are anticipated, such as in patients with trismus, restricted neck movement, or significant airway swelling14.
Anesthetic agents that induce general anesthesia for surgical drainage displace the soft palate and epiglottis against the posterior pharyngeal wall, leading to complete blockage of the airway6 that DNI had already narrowed. The risk of complete airway collapse upon anesthesia induction makes awake intubation a safer option in selected cases.
Patient cooperation is essential for successful awake in- tubation. However, uncooperative patients with altered mental status or severe sepsis may not be ideal candidates for this technique. Relative contraindications include allergy to local anesthetics, inexperience of the performing anesthesiologist, and the presence of bleeding (e.g., hemoptysis or oral hemor- rhage) or foreign bodies (e.g., vomitus or excessive secretions) in the airway that prevent glottic visualization using a fiber- optic bronchoscope (FOB)15. If a tracheal tube is to be inserted through a nostril, there must be no evidence of a basal skull defect, as this could result in intracranial placement of the tube. The only absolute contraindication is patient refusal. Preoperative imaging, including computed tomography (CT) scans, can provide valuable information regarding the extent of airway involvement and aid in decision-making7.
COMPARISON OF AWAKE TRACHEAL INTUBATION TECHNIQUES
Other awake tracheal intubation methods exist besides FBAI, such as using a videolaryngoscope alone or in conjunction with a FOB. Furthermore, a front-of-neck airway (FONA) may be inserted in awake patients when required. However, no single technique is recognized as the best for airway management in patients with DNI since each offers unique benefits and drawbacks.
1. Fiberoptic bronchoscopy-guided awake nasotracheal intubation (FBAI)
Although its success rate is very high16 with a 99% success rate reported in one prospective study17, FBAI requires ad- vanced skills18, sufficient clinical experience19, and consider- able time to complete the procedure20, contributing to a prolonged learning curve21. In addition, introducing a tracheal tube via the nasal cavity may cause epistaxis22, potentially impairing visualization during bronchoscope advancement. However, FBAI is favored for patients who have restricted mouth opening, an enlarged tongue, or a permanently flexed position of the neck16.
2. Awake intubation with videolaryngoscopy
Compared to FBAI, using a videolaryngoscope is easier to learn due to its short learning curve20 and consequently has a comparably high success rate of 98.3%20. As a result, intu- bation typically takes less time with videolaryngoscopy com- pared to FBAI20. Videolaryngoscopy provides a broader and more detailed view of the airway and surrounding structures than FBAI23. Although FBAI mandates using a tracheal tube with an internal diameter that exceeds the outer diameter of a FOB, resulting in limited tube size options, videolaryngoscopy permits a broader variety of tracheal tube sizes compared to FBAI20. If the chosen tracheal tube size is excessively large for the glottic opening, it can be swiftly swapped for a smaller one during videolaryngoscopy. However, in the case of FBAI, altering the tube size necessitates removing both the tracheal tube and the FOB.
However, videolaryngoscopy is not suitable for patients with limited mouth opening (e.g., trismus)16. This prevents the videolaryngoscope blade from being inserted into the oral cavity. Furthermore, manipulating the blade can trigger a gag reflex because of the pressure applied to the tongue. However, the FOB utilized in FBAI interacts more softly with the oropharyngeal structures, greatly lessening the chance of provoking a gag reflex during the procedure24.
3. Videolaryngoscope-assisted fiberoptic bronchoscopy-guided awake intubation
If FBAI or awake intubation with videolaryngoscopy is un- successful, a videolaryngoscope can serve as an additional tool to enhance the view of the larynx by moving the epi- glottis, which increases the chances of successful FBAI15,25-30. Manipulating the videolaryngoscope blade creates sufficient space for the tracheal tube mounted over the FOB to pass through a constricted airway. This method improves the view of the glottic opening and could potentially lessen airway trauma31.
This method necessitates 2 skilled operators: one to manage the videolaryngoscope and the other to control the FOB placed within the tracheal tube's lumen15.
4. Awake front-of-neck airway (awake FONA)
FONA is often viewed as a final option for airway manage- ment when traditional intubation methods are unsuccessful or unsafe16. In exceptional and carefully chosen situations, FONA may be executed on awake patients when alternative intubation methods are not feasible due to distorted anatomy, severe trismus, or rapidly progressing airway obstruction32. Conducting FONA in conscious patients demands thorough preparation, specialized expertise, and attentive patient col- laboration, since it can be both unsettling and technically demanding32. Methods like percutaneous cricothyroidotomy or tracheotomy with local anesthesia are typically used in these cases16,32. This technique is designated for specific cases and must be conducted by experienced clinicians in a controlled environment with full preparation for airway rescue.
TECHNIQUES FOR FIBEROPTIC BRONCHOSCOPY-GUIDED AWAKE NASOTRACHEAL INTUBATION
The following key steps are essential for an effective and safe FBAI.
1. Monitoring
Before starting the procedure, standard monitoring tech- niques like pulse oximetry, noninvasive blood pressure, and electrocardiogram should be in place33. Keeping track of patients' vital signs lowers the chances of complications by notifying medical practitioners34 (e.g., airway obstruction and hypoventilation due to oversedation, systemic effects of topical anesthetic or sedatives [hypotension or cardiac dysrhythmia]).
2. Oxygenation
To prevent or delay desaturation, supplemental oxygen must be administered as soon as the patient arrives in the operating room and should continue throughout the pro- cedure. High-flow nasal oxygen is preferred because it pro- vides apneic ventilation and continuous positive pressure, making it superior to low-flow devices like nasal cannulas or face masks17. The rate of desaturation (defined as peripheral oxygen saturation ≤90%) is significantly lower when high-flow nasal oxygen is utilized compared to low-flow devices (0~1.5% vs. 12~16%)16.
3. Premedication
After evaluating the relevant anatomy and nasal struc- tures, the side of the nasal opening designated for FBAI is identified35 and then topical nasal vasoconstrictors are applied to the chosen nasal cavity to minimize the risk of epistaxis during the insertion of a tracheal tube through the nasal cavity36. In our institution, we place cotton balls soaked in 0.1% epinephrine in the nasal cavity for 5 minutes before removing them. Antisialagogue agents, like glycopyrrolate (0.2~0.4 mg) or atropine (0.4~0.6 mg), are administered at least 20 minutes before FBAI, as their onset time is approximately 20 minutes16. These agents decrease secretions, enhancing the effectiveness and duration of topical anesthesia while aiding in airway visualization through FOB37. When taking these medications, it is essential to consider their systemic effects, such as tachycardia and dysrhythmias15.
4. Topical anesthesia
Topicalization of the airway is achieved using mucosal atomization, nebulization, or transtracheal injection of a local anesthetic15,38. Local anesthetic is delivered via the working channel of a FOB as it moves through the airway, utilizing the spray-as-you-go method. In our facility, we apply 10% lidocaine to the oropharynx and nasopharynx before placing a tracheal tube. When the FOB tip reaches the glottic opening, we administer 1~2 ml of 4% lidocaine through the working channel directed at the vocal cords to reduce the vocal cord reflex triggered by the FOB passing through the glottic entrance. It is essential to be aware that local anesthetic spread to the vocal cords may cause coughing. If the superficial anatomy over the cricothyroid membrane is palpable, we inject 3 ml of 4% lidocaine through the cricothyroid membrane directly into the tracheal lumen. The cough response helps to disperse the local anesthetic (nebulization), numbing the surrounding tissues in the air- way, including the vocal cords. Alternatively, the superior laryngeal and/or glossopharyngeal nerves can be blocked15. The maximum dose of topical lidocaine must not surpass 9 mg/kg of lean body weight39, which is rarely required. However, medical practitioners should be alert to the devel- opment of systemic toxicity when using local anesthetics, regardless of the administration technique used40,41.
5. Sedation
If topical anesthesia is appropriate and patients cooperate with medical personnel and tolerate the procedure, sedation is not mandatory for the safe and effective performance of FBAI17,38. Nonetheless, it provides anxiolysis and comfort and increases tolerance during the procedure42. However, there is a risk of oversedation, which might lead to respiratory de- pression or airway obstruction, potentially resulting in asphyxia or cardiovascular instability. Therefore, independent medical personnel should deliver sedation while monitoring the vital signs to enhance the advantages of sedation and minimize the chances of side effects or complications16.
Remifentanil and dexmedetomidine are widely used for FBAI because of the low risk of airway obstruction resulting from oversedation42. Remifentanil is a potent, ultra-short-acting μ-opioid receptor agonist with a context-sensitive half-time of 3 minutes and an elimination half-life of 6 minutes. These characteristics result from its rapid hydrolysis by nonspecific tissue and plasma esterase. It aids in tracheal intubation by delivering profound analgesia and suppressing airway reflexes, while having little impact on cognitive function43. The Minto pharmacokinetic model is used to administer remifentanil to maintain the target effect-site concentrations between 1 and 3 ng/ml16,44,45. Remifentanil can cause bradycardia, hypotension, apnea, and chest wall rigidity, but its effects can be reversed with naloxone.
Dexmedetomidine induces physiologic sleep without causing respiratory depression and provides potent analgesic effects by activating α2-adrenergic receptors located in the locus coeruleus and the spinal cord, respectively46. However, acti- vating post- and pre-synaptic α2 receptors in the central and peripheral nervous system results in bradycardia and hypoten- sion. Conversely, its bolus administration causes hypertension by activating α2 receptors in the vascular tissue. Following bolus administration at doses of 0.5~1 μg/kg over 5 minutes, it is continuously infused at doses of 0.3~0.6 μg/kg/hr16.
6. Performance of fiberoptic bronchoscope-guided awake nasotracheal intubation
When sedatives and supplemental oxygen are being admin- istered continuously following premedication and topical anesthesia, FBAI is prepared to commence. If patients cannot tolerate the supine position, FBAI may be conducted with them seated in the Fowler's position or upright11. Once the more patent nostril is expanded using a nasopharyngeal airway with an internal diameter of 6~7 mm, a cuffed tracheal tube with an internal diameter of 6.5 mm (for women) or 7 mm (for men) is inserted into the nasal cavity at a 90° angle to the face along the nasal floor by a specified distance (between the nasal tip and the external auditory opening)47.
A FOB is placed into the lumen of the tracheal tube and advanced past the tube tip to reach the glottic opening be- neath the epiglottis. The gag reflex, involuntary swallowing or coughing, and excess secretions can hinder clear visualization of the anatomical structures of interest. Adjustments such as moving the FOB tip up and down with the control lever, rotating the FOB body, or using the built-in suction port to clear secretions may be necessary to improve the view of the glottic opening. A local anesthetic is sprayed toward the vocal cords to minimize the vocal cord reflex caused by the FOB tip passing through the glottic opening. If the vocal cords remain functional and their closure inhibits the FOB from passing despite the spray-as-you-go technique or transtracheal injection of local anesthetic, advancing the FOB tip during the patient's inspiration can facilitate its smooth entry into the trachea. Once the FOB tip crosses the glottic opening, the tracheal rings become visible, and further advancement enables identification of the carina.
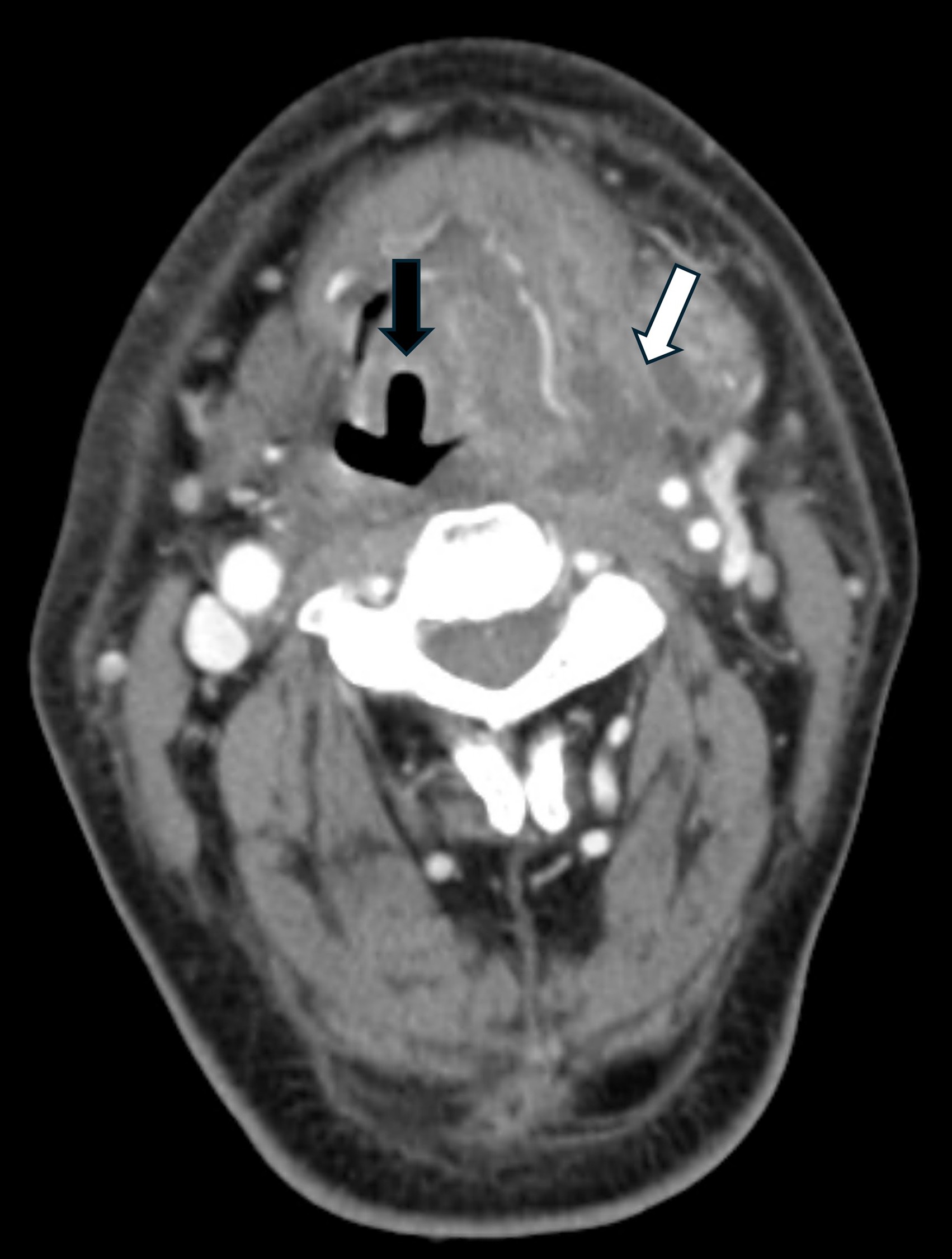
The tracheal tube, already positioned above the glottic opening, is turned 90° counterclockwise to align closely with the insertion cord of the FOB48 and then advanced over the insertion cord into the trachea when the patient inhales. After confirming with the FOB that the tracheal tube tip is positioned between the vocal cords and the carina, the FOB is withdrawn, and the cuff is gently inflated. Once the tracheal tube connector is attached to the Y-piece of the breathing circuit, the correct placement of the tracheal tube in the airway should be confirmed by the appearance of the capnographic waveform. Anesthesia should be induced promptly upon confirmation of the proper tracheal tube placement. In cases of a pharyngeal wall abscess, it is crucial to handle the FOB and tracheal tube with extreme caution due to the potential risk of abscess rupture and subsequent aspiration of pus8. A notable FBAI performance for a patient, indicated by pre- operative CT revealing an airway deviation from the anatomical midline caused by a left parapharyngeal abscess (Fig. 1), is showcased in a video clip provided in the journal website. (Click here)
UNSUCCESSFUL AWAKE INTUBATION
While awake intubation is the preferred method for airway management in DNI patients, other strategies must be con- sidered in cases where awake intubation is not feasible or has failed. According to recent Difficult Airway Society guidelines16, unsuccessful awake tracheal intubation is characterized by 4 consecutive failed attempts, during which the FOB or tracheal tube is unintentionally removed from the airway. The same medical practitioner conducts the initial 3 attempts, while the final attempt should involve a more experienced one.
In case of unsuccessful awake tracheal intubation, the medical practitioner should immediately call for help, ensure that 100% oxygen is administered, and cease or reverse sedation. When the procedure cannot be delayed, such as in cases of compromised airway patency, impaired ventilation, altered neurological status, the requirement for urgent or emergent surgeries, or anticipated clinical deterioration, awake cricothyroidotomy or tracheotomy becomes a preferred option. This approach necessitates favorable anatomy, patient compliance, a proficient surgical and anesthesia team, and suitable equipment, while also posing risks for bleeding, infection, and subcutaneous emphysema49.
Due to the potential risk for total airway collapse during anesthesia induction, tracheal intubation under general anesthesia should be regarded as a last resort if the awake surgical airway is unsuccessful. The most skilled medical practitioner must perform the intubation using a video- laryngoscope, with the surgical airway ready in case of failed intubation.
EMERGING TECHNOLOGIES AND FUTURE DIRECTIONS
Recent advancements in airway management include the use of airway assessment tools with three-dimensional (3D) printed airway models and artificial intelligence50. 3D airway models can be created from two-dimensional images and associated data. This method offers accurate representations of the anatomical structures of the airway and the bio- mechanics of intubation, assisting medical practitioners in developing the safest plan for managing difficult airway51-55. Artificial intelligence algorithms can predict difficult airways and suggest optimal management strategies based on imaging and clinical parameters50. Future research should focus on refining and integrating these technologies into clinical practice to enhance airway management in patients with DNI.
DNIs pose significant challenges in airway management because of anatomical distortions caused by soft tissue swell- ing and abscess formation, raising the likelihood of airway obstruction. Therefore, FBAI is the recommended method, providing airway security while allowing spontaneous breath- ing. This approach avoids the risks associated with general anesthesia induction, which may result in total airway collapse. In conclusion, suitable airway management strategies are essential in minimizing the morbidity and mortality associated with DNIs.
References
1. Craig FW, Schunk JE. Retropharyngeal abscess in children: clinical presentation, utility of imaging, and current management. Pediatrics 2003;111:1394-1398
Google Scholar
2. Wang B, Gao BL, Xu GP, Xiang C. Images of deep neck space infection and the clinical significance. Acta Radiol 2014;55:945-951
Google Scholar
3. Abdel-Haq NM, Harahsheh A, Asmar BL. Retropharyngeal abscess in children: the emerging role of group A beta hemolytic streptococcus. South Med J 2006;99:927-931
Google Scholar
4. Philpott CM, Selvadurai D, Banerjee AR. Paediatric retro- pharyngeal abscess. J Laryngol Otol 2004;118:919-926
Google Scholar
5. Karkos PD, Leong SC, Beer H, Apostolidou MT, Panarese A. Challenging airways in deep neck space infections. Am J Otolaryngol 2007;28:415-418
Google Scholar
6. Nandi PR, Charlesworth CH, Taylor SJ, Nunn JF, Dore CJ. Effect of general anaesthesia on the pharynx. Br J Anaesth 1991;66:157-162
Google Scholar
7. Cho SY, Woo JH, Kim YJ, Chun EH, Han JI, Kim DY, et al. Airway management in patients with deep neck infections: A retrospective analysis. Medicine (Baltimore) 2016;95: e4125
Google Scholar
8. Vieira F, Allen SM, Stocks RM, Thompson JW. Deep neck infection. Otolaryngol Clin North Am 2008;41:459-483
Google Scholar
9. Bross-Soriano D, Arrieta-Gomez JR, Prado-Calleros H, Schimelmitz-Idi J, Jorba-Basave S. Management of Ludwig's angina with small neck incisions: 18 years experience. Otolaryngol Head Neck Surg 2004;130:712-717
Google Scholar
10. Wasson J, Hopkins C, Bowdler D. Did Ludwig's angina kill Ludwig? J Laryngol Otol 2006;120:363-365
Google Scholar
11. Ovassapian A, Tuncbilek M, Weitzel EK, Joshi CW. Airway management in adult patients with deep neck infections: a case series and review of the literature. Anesth Analg 2005;100:585-589
Google Scholar
12. Murphy P. A fibre-optic endoscope used for nasal in- tubation. Anaesthesia 1967;22:489-491
Google Scholar
13. Apfelbaum JL, Hagberg CA, Connis RT, Abdelmalak BB, Agarkar M, Dutton RP, et al. 2022 American Society of Anesthesiologists practice guidelines for management of the difficult airway. Anesthesiology 2022;136:31-81
Google Scholar
14. Crawley SM, Dalton AJ. Predicting the difficult airway. BJA Educ 2015;15:253-257
Google Scholar
15. Vora J, Leslie D, Stacey M. Awake tracheal intubation. BJA Educ 2022;22:298-305
Google Scholar
16. Ahmad I, El-Boghdadly K, Bhagrath R, Hodzovic I, McNarry AF, Mir F, et al. Difficult Airway Society guidelines for awake tracheal intubation (ATI) in adults. Anaesthesia 2020;75:509-528
Google Scholar
17. El-Boghdadly K, Onwochei DN, Cuddihy J, Ahmad I. A prospective cohort study of awake fibreoptic intubation practice at a tertiary centre. Anaesthesia 2017;72:694-703
Google Scholar
18. Fitzgerald E, Hodzovic I, Smith AF. 'From darkness into light': time to make awake intubation with video- laryngoscopy the primary technique for an anticipated difficult airway? Anaesthesia 2015;70:387-392
Google Scholar
19. Allan AG. Reluctance of anaesthetists to perform awake intubation. Anaesthesia 2004;59:413
Google Scholar
20. Alhomary M, Ramadan E, Curran E, Walsh SR. Video- laryngoscopy vs. fibreoptic bronchoscopy for awake tracheal intubation: a systematic review and meta-analysis. Anaesthesia 2018;73:1151-1161
Google Scholar
21. Dalal PG, Dalal GB, Pott L, Bezinover D, Prozesky J, Bosseau Murray W. Learning curves of novice anesthesi- ology residents performing simulated fibreoptic upper airway endoscopy. Can J Anaesth 2011;58:802-809
Google Scholar
22. Heidegger T, Gerig HJ, Ulrich B, Schnider TW. Structure and process quality illustrated by fibreoptic intubation: analysis of 1,612 cases. Anaesthesia 2003;58:734-739
Google Scholar
23. Jeyadoss J, Nanjappa N, Nemeth D. Awake intubation using Pentax AWS videolaryngoscope after failed fibre- optic intubation in a morbidly obese patient with a massive thyroid tumour and tracheal compression. Anaesth Intensive Care 2011;39:311-312
Google Scholar
24. McKenna JR, Ball DR. Awake nasal intubation: the gag reflex and failure of videolaryngoscopy. Anaesthesia 2015;70:879-880
Google Scholar
25. Khan MF, Shamim F, Slote MU, Salim B, Abbas SA. Combined use of a videolaryngoscope and a flexible bronchoscope for awake tracheal intubation when front-of-neck airway is not an option. Anaesth Rep 2021;9:12-15
Google Scholar
26. Kim SM, Kim HJ. Successful advancement of endotracheal tube with combined fiberoptic bronchoscopy and video- laryngoscopy in a patient with a huge goiter. SAGE Open Med Case Rep 2020;8:2050313X20923232
Google Scholar
27. Gomez-Rios MA, Nieto Serradilla L. Combined use of an Airtraq® optical laryngoscope, Airtraq video camera, Airtraq wireless monitor, and a fibreoptic bronchoscope after failed tracheal intubation. Can J Anaesth 2011;58: 411-412
Google Scholar
28. Lenhardt R, Burkhart MT, Brock GN, Kanchi-Kandadai S, Sharma R, Akca O. Is video laryngoscope-assisted flexible tracheoscope intubation feasible for patients with pre- dicted difficult airway? A prospective, randomized clinical trial. Anesth Analg 2014;118:1259-1265
Google Scholar
29. Koopman EM, van Emden MW, Geurts JJG, Schwarte LA, Schober P. Comparison of videolaryngoscopy alone with video-assisted fibreoptic intubation in a difficult cadaver airway model. Eur J Anaesthesiol 2021;38:318-319
Google Scholar
30. Sanfilippo F, Chiaramonte G, Sgalambro F. Video laryngo- scopes and best rescue strategy for unexpected difficult airways: Do not forget a combined approach with flexible bronchoscopy! Anesthesiology 2017;126:1203
Google Scholar
31. Sgalambro F, Sanfilippo F, Santonocito C, Caltavuturo C, Grillo C. Virtual laryngoscopy and combined laryngoscopic-bronchoscopic approach for safe manage- ment of obstructive upper airways lesions. Br J Anaesth 2014;113:304-306
Google Scholar
32. Warwick E, Yoon S, Ahmad I. Awake tracheal intubation: An update. Int Anesthesiol Clin 2024;62:59-71
Google Scholar
33. Klein AA, Meek T, Allcock E, Cook TM, Mincher N, Morris C, et al. Recommendations for standards of monitoring during anaesthesia and recovery 2021: Guideline from the Association of Anaesthetists. Anaesthesia 2021;76: 1212-1223
Google Scholar
34. McKay WP, Noble WH. Critical incidents detected by pulse oximetry during anaesthesia. Can J Anaesth 1988; 35:265-269
Google Scholar
35. Kumar A, Gupta A, Gupta N, Bhargava T, Kumar V. In reply: Comparing approaches to the difficult airway. Can J Anaesth 2024;71:1181-1182
Google Scholar
36. Song J. A comparison of the effects of epinephrine and xylometazoline in decreasing nasal bleeding during nasotracheal intubation. J Dent Anesth Pain Med 2017; 17:281-287
Google Scholar
37. Brookman CA, Teh HP, Morrison LM. Anticholinergics improve fibreoptic intubating conditions during general anaesthesia. Can J Anaesth 1997;44:165-167
Google Scholar
38. Sandefur BJ, Driver BE, Long B. Managing awake in- tubation. Ann Emerg Med 2025;85:21-30
Google Scholar
39. Ingrande J, Lemmens HJ. Dose adjustment of anaesthetics in the morbidly obese. Br J Anaesth 2010;105 Suppl 1: i16-23
Google Scholar
40. Wiles JR, Kelly J, Mostafa SM. Hypotension and brady- cardia following superior laryngeal nerve block. Br J Anaesth 1989;63:125-127
Google Scholar
41. Woodall NM, Harwood RJ, Barker GL. Complications of awake fibreoptic intubation without sedation in 200 healthy anaesthetists attending a training course. Br J Anaesth 2008;100:850-855
Google Scholar
42. Johnston KD, Rai MR. Conscious sedation for awake fibreoptic intubation: a review of the literature. Can J Anaesth 2013;60:584-599
Google Scholar
43. Burkle H, Dunbar S, Van Aken H. Remifentanil: a novel, short-acting, mu-opioid. Anesth Analg 1996;83:646-651
Google Scholar
44. Minto CF, Schnider TW, Shafer SL. Pharmacokinetics and pharmacodynamics of remifentanil. II. Model application. Anesthesiology 1997;86:24-33
Google Scholar
45. Minto CF, Schnider TW, Egan TD, Youngs E, Lemmens HJ, Gambus PL, et al. Influence of age and gender on the pharmacokinetics and pharmacodynamics of remifentanil. I. Model development. Anesthesiology 1997;86:10-23
Google Scholar
46. Gerlach AT, Dasta JF. Dexmedetomidine: an updated review. Ann Pharmacother 2007;41:245-252
Google Scholar
47. Kumar A, Gupta N, Bhargava T, Gupta A, Kumar V, Bharti SJ, et al. A comparative evaluation of fibreoptic bronchoscopy versus C-MAC® D-BLADE-guided video- laryngoscopy for nasotracheal intubation under general anesthesia in oropharyngeal carcinoma surgery patients. Can J Anaesth 2024;71:503-510
Google Scholar
48. Asai T, Shingu K. Difficulty in advancing a tracheal tube over a fibreoptic bronchoscope: incidence, causes and solutions. Br J Anaesth 2004;92:870-881
Google Scholar
49. Zasso FB, You-Ten KE, Ryu M, Losyeva K, Tanwani J, Siddiqui N. Complications of cricothyroidotomy versus tracheostomy in emergency surgical airway management: a systematic review. BMC Anesthesiol 2020;20:216
Google Scholar
50. Chen H, Zheng Y, Fu Q, Li P. A review of the current status and progress in difficult airway assessment research. Eur J Med Res 2024;29:172
Google Scholar
51. Ormandy D, Kolb B, Jayaram S, Burley O, Kyzas P, Vallance H, et al. Difficult airways: a 3D printing study with virtual fibreoptic endoscopy. Br J Oral Maxillofac Surg 2021;59: e65-e71
Google Scholar
52. Kovatch KJ, Powell AR, Green K, Reighard CL, Green GE, Gauger VT, et al. Development and multidisciplinary preliminary validation of a 3-dimensional-printed pediatric airway model for emergency airway front-of-neck access procedures. Anesth Analg 2020;130:445-451
Google Scholar
53. Han B, Liu Y, Zhang X, Wang J. Three-dimensional printing as an aid to airway evaluation after tracheotomy in a patient with laryngeal carcinoma. BMC Anesthesiol 2016; 16:6
Google Scholar
54. Ahmad I, Millhoff B, John M, Andi K, Oakley R. Virtual endoscopy--a new assessment tool in difficult airway management. J Clin Anesth 2015;27:508-513
Google Scholar
55. Zhang X, Wang J, Liu Y, Li Z, Han B. A rare case of an unexpected difficult airway management in a diffuse idiopathic skeletal hyperostosis patient and post-operative airway evaluation with 3D printing technique. Ann Transl Med 2021;9:75
Google Scholar
Congratulatory MessageClick here!