pISSN : 3058-423X eISSN: 3058-4302
Open Access, Peer-reviewed

pISSN : 3058-423X eISSN: 3058-4302
Open Access, Peer-reviewed
Shivaali A,Moby Saira Luke,John Maria Louis,Priyadarshini Shanmugam
10.17966/JMI.2024.29.4.200 Epub 2025 January 03
Abstract
We report a case of haemopneumothorax complicated by Chryseobacterium indologenes infection in a 76-year-old male patient who sustained injuries to the left thigh and right chest. His past medical illnesses included chronic obstructive pulmonary disease and coronary artery disease (CAD), and he had a personal history of chronic smoking and alcohol consumption. The examination findings included an active lacerated wound on the left thigh and paradoxical breathing with tenderness over the right chest. Emergency wound exploration revealed a grade IV muscle tear of the vascular medialis and further evaluation revealed Type II respiratory failure, flail chest, right subcutaneous emphysema, haemopneumothorax and multiple rib fractures. Treatment involved the insertion of an intercostal drainage tube on day 3 and the administration of empirical antibiotics and other supportive medications. The isolation of C. indologenes highlights the challenge of managing infectious complications in traumatic haemopneumothorax, particularly in patients with underlying respiratory comorbidities. A multidisciplinary approach is essential to optimize outcomes in such complicated cases.
Keywords
Chronic obstructive pulmonary disease Chryseobacterium indologenes Healthcare-associated infections Haemopneumothorax Respiratory failure Road traffic accident
Chryseobacterium indologenes is an opportunistic pathogen, significant in healthcare settings due to its association with infections in immunocompromised individuals. It is known for its intrinsic resistance to many antibiotics such as carbapenems and colistin. This highlights the necessity to establish prompt and accurate detection in laboratories to guide appropriate treatment strategies1. The bacterium causes a variety of infections, including pneumonia, bacteremia, and urinary tract infections, especially in patients with indwelling medical devices. Its ability to form biofilms contributes to its persistence in hospital environments and medical equipment. Understanding and monitoring this organism is crucial for preventing nosocomial infections and improving patient outcomes. This rare case report sheds light on the emergence of uncommon pathogens such as C. indologenes in clinical settings. It also emphasizes the critical role of antimicrobial stewardship and underscores the challenges in managing nosocomial infections in the context of traumatic haemopneumothorax, particularly in patients with pre-existing respiratory conditions and a history of chronic smoking and alcohol consumption. In addition, efforts to mitigate the risk factors for traumatic injuries and prevent nosocomial infections are crucial for the reduction of morbidity and mortality associated with such cases.
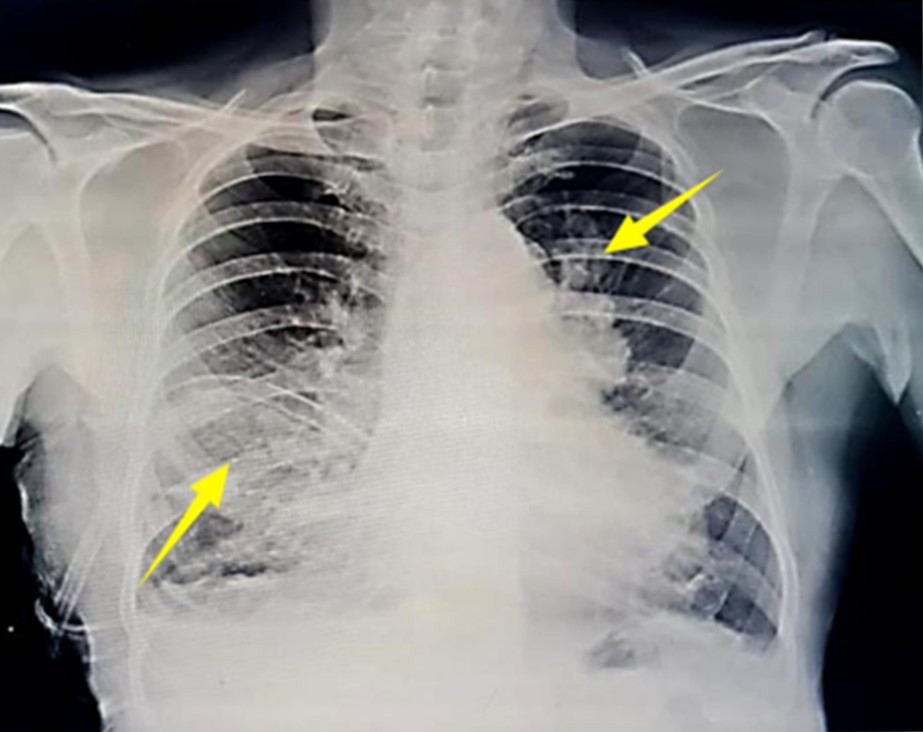
A 76-year-old male patient reported to the emergency medicine department after a road traffic accident between the two-wheeler vehicle he was riding and a stationary vehicle. He sustained injuries to the inner aspect of his left thigh and right side of his chest. Initial management at a nearby hospital included tagging and suturing of a muscle tear in the left thigh. The pain on the right side of his chest was not associated with breathlessness, abdominal pain, loss of consciousness, head injury, ENT bleeding, nausea or vomiting. His past medical history included coronary artery disease for which he had received treatment for 5 years and chronic obstructive pulmonary disease 10 years ago, for which he was on intermittent nebulization and used budamate via a metered-dose inhaler. He had >20 years of smoking and alcohol consumption history but stopped both 8 years ago. He had no history of COVID-19 or any other significant medical conditions. Upon examination, approxi- mately 50 mL of clot was accompanied with a laceration measuring 6 × 3 × 2 cm over the inner aspect of the left thigh just above the medial condyle. Active diffuse bleeding and tenderness were observed. In the right chest, paradoxical breathing, tenderness and subcutaneous emphysema were noted. His blood pressure was 190/100 mmHg, with a pulse rate of 90 beats per minute. The respiratory rate was at 24 breaths per minute and examination of the chest indicated reduced bilateral air entry, fine crepitations and bilateral wheezing. During hospitalization, consultations were sought from a surgeon and a pulmonologist. Further examinations revealed fractures of the 4th, 5th, and 6th ribs along with a grade IV muscle tear2 of the vastus medialis. Emergency wound exploration revealed the extent of the injuries. The patient was started empirically on broad-spectrum antibiotics intravenously twice daily with injections of piperacillin + tazobactam 4.5 g, metronidazole 500 mg, amikacin 500 mg and other supportive medications. Imaging studies, including chest X-ray imaging (Fig. 1) and high-resolution computed tomography of the chest, revealed significant thoracic injuries such as displaced fracture of the 5th rib in the anterolateral aspect, undisplaced fracture of the 6th rib, minimal haemo- pneumothorax of the right side, and a lobulated mediastinal mass measuring 5.3 × 5.1 cm in the left upper lobe, prompt- ing further evaluations. Echocardiography did not detect regional wall motion abnormalities with normal left ventricular systolic function with an ejection fraction of 60%. Echo- cardiography incidentally found grade I diastolic dysfunction, concentrated left ventricular hypertrophy, aortic valve sclerosis and trivial tricuspid regurgitation with normal pulmonary arterial pressure. No clots or vegetations were found and the patient was transferred to the intensive care unit due to type II respiratory failure and an intercostal drainage tube was inserted for the management of the haemopneumothorax. His initial blood results showed a hemoglobin level of 10.6 gm/dL, total cell count of 15,600 cells/μL, differential count of 80.5% of neutrophils, 8.3% of lymphocytes, 4.4% of eosino- phils, 0.1% of basophils and platelet count of 2.91 lakh/μL. No biochemical analysis of the pleural fluid was performed. His routine urine examination showed straw-colored urine, with a specific gravity of 1.025 and no urinary sugars, ketone bodies, bile salts, or bile pigments were present. Urinary leucocyte esterase and urinary nitrates were negative. Pleural fluid samples for culture and sensitivity were sent on day 8 (April 23, 2024). Gram staining revealed moderate pus cells with a few Gram-negative bacilli. It was directly inoculated into blood agar, chocolate agar and MacConkey agar and they were aerobically incubated at 35℃ ± 2℃ for 18~24 h. The next day, colonies were observed on the blood agar (Fig. 2) and chocolate agar (Fig. 3), appearing as circular, lowly convex, smooth-edged, and approximately 1~2 mm in diameter, and yellow-colored colonies that also exhibited deep beta-haemolytic (on blood agar) mucoid colony characteristics that turned red upon decanting with 10% KOH. MacConkey agar showed small lactose non-fermenting colonies (Fig. 4). Further, on Gram staining of the colonies showed uniformly stained Gram-negative bacilli. The catalase and oxidase tests yielded positive results and the organisms were nonmotile when tested using the hanging drop method. The bile esculin test returned negative. Biochemical testing indicated that the indole test was positive and the triple sugar iron agar exhibited an alkaline slant with an alkaline butt without gas or H2S formation. Citrate was not utilized, urea was not hydrolyzed, mannitol was not fermented, there was no motility, nitrate was reduced to nitrite, the DNase agar showed a clear zone surrounding the colonies and the phenylalanine agar tested negative. A Flavobacterium species was initially identified; subsequently, VITEK 2 compact automated Iden- tification systems and conventional biochemical methods confirmed it as Chryseobacterium indologenes with 97% probability. Antimicrobial susceptibility testing was performed using VITEK 2 automated compact systems and by the Kirby-Bauer disc diffusion method aerobically at 35℃ ± 2℃ for 18~24 hours on Mueller-Hinton agar medium. The results demonstrated susceptibility to cotrimoxazole and resistance to levofloxacin, cefepime, ceftazidime, imipenem, mero- penem, amikacin, gentamicin, ciprofloxacin and piperacillin-tazobactam. To interpret the antimicrobial susceptibility data, the Clinical and Laboratory Standards Institute Guidelines (2024) were followed categorically using the breakpoint guidelines for non-Enterobacteriaceae and Pseudomonas aeruginosa as points of reference3,4. Antibiotic therapy was then changed to intravenous injection of ceftriaxone 1 gm twice daily along with cotrimoxazole 800/160 mg one tablet twice daily as per the antimicrobial susceptibility testing, which resulted in the clinical improvement and eventually the removal of the intercostal drainage tube on day 15. Subsequent blood counts showed improvement, and no growth was found on sputum and pleural fluid cultures, indicating the resolution of the impending infection.



Haemopneumothorax causes the accumulation of blood and air in the pleural cavity and typically arises from traumatic chest injuries that disrupt the lung tissue and adjacent blood vessels5. This accumulation compromises lung expansion and ventilation, predisposing patients to respiratory distress and infections5. The diagnosis of coexisting infection can be challenging because of the need for specialized techniques to isolate the organism from pleural fluid cultures. Patients with underlying conditions such as chronic obstructive pulmonary disease and CAD face heightened risk of infections that are intensified by factors such as chronic smoking and alcohol consumption. Similar case reports from other countries are presented in Table 1.
|
Author |
Institute/ Country |
Year |
Age/Sex |
Pre
disposing |
Sample sent |
Outcome |
|
Arif et al.7 |
AIIMS,
New Delhi, |
2019 |
42/Male
|
Pleural effusion with aortic |
Pleural
fluid |
Recovered |
|
Soydan |
Bahcesehir
University |
2017 |
69/Male |
Elderly male with chronic |
Sputum |
Improved |
|
Monteen |
UTHSC,
Memphis, |
2013 |
66/Male |
Elderly male trauma patient |
Broncho |
Recovered |
C. indologenes, once primarily found environmentally, has emerged as a nosocomial pathogen with intrinsic antibiotic resistance and a tendency to form biofilms on medical devices such as indwelling catheters. Its ability to colonize medical devices and health care settings raises concerns, necessitating stringent infection control measures10. It was found to cause many other diseases such as meningitis, pyomyositis, keratitis, pneumonia, and bacteremia and contamination of surgically implanted devices11. These features make it a potentially dangerous pathogen. The diagnosis of C. indologenes in- fection requires specialized microbiological techniques and its treatment often involves broad-spectrum antibiotics adjusted based on culture results12. Intensive care unit management may be necessary for patients with severe respiratory com- promise, emphasizing the importance of multidisciplinary care involving expertise in traumasurgery, pulmonary, infectious disease and critical care. Successful resolution of infection and removal of drainage tubes signal a positive prognosis; however, long-term follow-up is crucial13. Further studies are needed to refine management strategies, particularly for older patients with multiple comorbidities and immuno- compromised status. Understanding the epidemiology and antibiotic resistance patterns of C. indologenes is vital for guiding treatment decisions and improving outcomes6. Overall, this case underscores the complexities of managing haemopneumothorax complicated by infection and the need for comprehensive and collaborative care.
References
1. Chang J, Kim S, Kwak YG, Um TH, Cho CR, Song JE. Clinical and Microbiological Characteristics of Chryseo- bacterium indologenes Bacteremia: A 20-Year Experience in a Single University Hospital. Infect Chemother 2023; 55:322-327
Google Scholar
2. Maffulli N, Oliva F, Frizziero A, Nanni G, Barazzuol M, Via AG, et al. ISMuLT Guidelines for muscle injuries. Muscles Ligaments Tendons J 2014;3:241-249
Google Scholar
3. CLSI M100 Ed34. Clinical & Laboratory Standards In- stitute. https://clsi.org/standards/products/microbiology/ documsents/m100/
4. Kirby JT, Sader HS, Walsh TR, Jones RN. Antimicrobial susceptibility and epidemiology of a worldwide collection of Chryseobacterium spp.: Report from the SENTRY Antimicrobial Surveillance Program (1997-2001). J Clin Microbiol 2004;42:445-448
Google Scholar
5. Chastre J, Fagon JY. Ventilator-associated pneumonia. Am J Respir Crit Care Med 2002;165:867-903
Google Scholar
6. Arif N, Khullar S, Kumar R, Choudhary SK, Kapil A, Dhawan B. Pleural effusion due to Chryseobacterium indologenes: Case report and review of literature. J Lab Physicians 2019; 11:284-286
Google Scholar
7. Soydan S, Ignak S, Unay Demirel O, Karadağ G, Aykent A, Aslan S. Chryseobacterium indologenes infection in a patient with chronic obstructive pulmonary disease. Drug Discov Ther 2017;11:165-167
8. Monteen MR, Ponnapula S, Wood GC, Croce MA, Swanson JM, Boucher BA, et al. Treatment of Chryseo- bacterium indologenes ventilator-associated pneumonia in a critically ill trauma patient. Ann Pharmacother 2013; 47:1736-1739
Google Scholar
9. Bacterial sepsis treatment & management [Internet]. Medscape.com. 2024 [cited 2024 Nov 29]. https:// emedicine.medscape.com/article/234587-treatment?form =fpf
Google Scholar
10. Ece G, Ocakci S, Cagirgan S. Chryseobacterium indo- logenes Pneumoniae in a patient with Acute Myeloid Leukemia. Indian Journal of Medical Case Reports 2013; 2:35-38
Google Scholar
11. Izaguirre-Anariba DE, Sivapalan V. Chryseobacterium indologenes, an emerging bacteria: A case report and review of literature. Cureus 2020;12:e6720
Google Scholar
12. Srinivasan G, Muthusamy S, Raveendran V, Joseph NM, Easow JM. Unforeseeable presentation of Chryseo- bacterium indologenes infection in a paediatric patient. BMC Res Notes 2016;9:212
Google Scholar
13. Hankenson KD, Dishowitz M, Gray C, Schenker M. Angio-genesis in bone regeneration. Injury 2011;42:556-561
Google Scholar
Congratulatory MessageClick here!