pISSN : 3058-423X eISSN: 3058-4302
Open Access, Peer-reviewed

pISSN : 3058-423X eISSN: 3058-4302
Open Access, Peer-reviewed
Alexander Mannu,Priyadarshini Shanmugam,Brihadishwaran Thiyagarajan
10.17966/JMI.2024.29.4.196 Epub 2025 January 03
Abstract
Bacillus Calmette-Guérin (BCG) vaccine, a live attenuated vaccine derived from Mycobacterium bovine, has been used as a part of routine immunization programs. One of the complications of this vaccination is BCG adenitis, which is the enlargement of the regional lymph node in the axillary or supraclavicular area. Normally, this condition resolves approximately 6 weeks after vaccination, and persistent BCG adenitis is rarely seen in children with immunocompetence. Herein, a 5-month-old boy presented with complaints of left axillary lymphadenopathy after 2 weeks of BCG vaccination. Ultrasonography revealed a nontender mobile lymph node measuring approximately 2.5 × 2 cm, which persisted beyond 12 months of age. The parents insisted on removing the swelling surgically at the age of 18 months as it did not resolve on its own. The lesion was removed and sent for HPE examination, acid-fast bacilli (AFB) staining, and GeneXpert for Mycobacterium tuberculosis (MTB). In the current case, the HPE revealed epithelioid cell granulomatous lesions, with no AFB or necrosis. The GeneXpert MTB/RIF (Cepheid) test was positive, which detected the MTB complex (including MTB and BCG), suggestive of BCG adenitis without active tuberculosis. This case shows that BCG adenitis can persist even beyond the age of 12 months. Careful history taking and timely adequate investigation along with the knowledge that GeneXpertMtb detects MTB complex will aid in the correct diagnosis.
Keywords
BCG adenitis BCG vaccine Immunization Lymphadenopathy Mycobacterium bovis Tuberculosis
Bacillus Calmette-Guérin (BCG) is a live attenuated vaccine prepared from Mycobacterium bovis with residual virulence to protect against tuberculosis (TB). It was first developed by Calmette and Guérin and approved for human use in 1921. This was the only vaccine against TB and is included as part of the routine immunization schedule in India1. BCG adenitis is a common complication of its vaccination, which occurs in infants aged 3 months or older and usually persists until 6 weeks after vaccination2. This occurs as a response to the BCG vaccine, causing the enlargement of the regional lymph nodes, with major involvement of the axillary (armpit) or supraclavicular (neck) nodes. These lymph nodes enlarge to their maximum size at around 3 months of age, and it is not a cause for alarm unless there is softening or cold abscess formation. This is a self-resolving condition, so no active inter- ventions are required2.
Herein, we report an interesting case of persistent non- suppurative adenitis in a baby with an immunocompetent status, who presented with axillary adenitis even after the age of 1.5 years.


A 5-month-old boy was brought by his parents to the pediatrician, with complaints of left axillary swelling for the past 2 weeks. He had BCG vaccination at birth, and his parents gave a history suggestive of the usual BCG reaction leading to a scar formation at the vaccination site. He had no history of contact with individuals diagnosed with TB. The patient had adequate weight gain for age and was on exclusive breast feeding, which was planned until 6 months of age. The developmental milestones were normal for his age.
On examination, the infant was active and alert and had a significantly enlarged left axillary lymph node measuring 2.5 × 2 cm, which was not tender, moderately mobile, and not fixed to underlying structures or skin, which was con- firmed by ultrasonography. The parents were counseled on the benign, self-limiting nature of the nodes and were asked to review if it had progressed or remained unresolved by the child's first birthday. On follow-up on his first birthday, the infant was healthy; however, the axillary node remained with no complications. This worried the parents, who were counseled again for observation and advised to follow-up every 3 months to check for progression or complications.
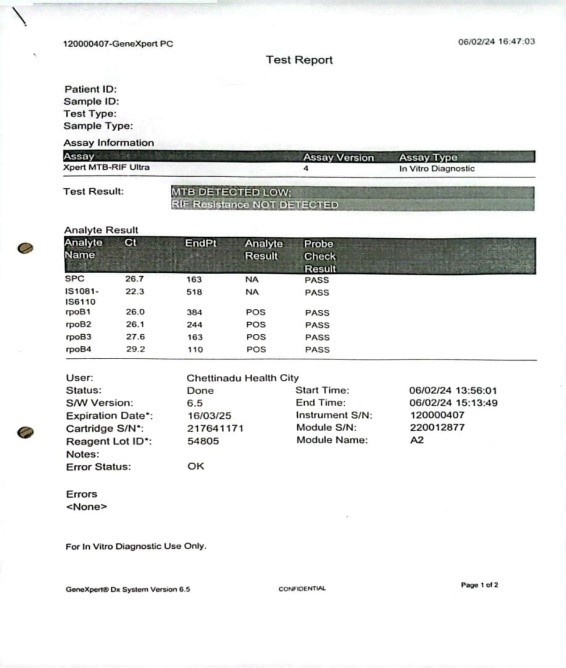
At the 18-month follow-up, the size of the left axillary lymph node was the same, with no complications, as confirmed by sonographic imaging. The parents insisted on the removal of the node. Thus, after the surgical consultation, the child underwent an excisional biopsy of the node. The node was excised and sent for HPE examination, Gram staining, acid-fast bacilli (AFB) staining, and GeneXpert for Mycobacterium tuberculosis (MTB).
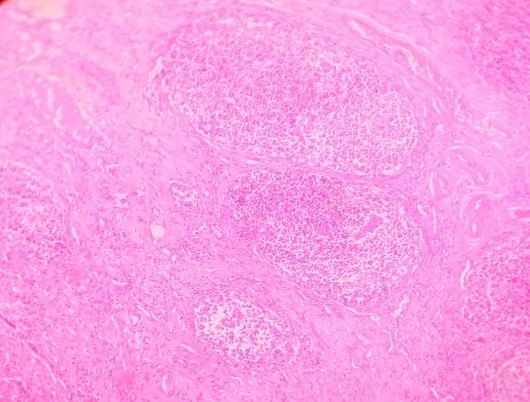
The Ziehl-Neelsen staining was non-contributory, and the GeneXpert was positive for MTB. HPE showed epithelioid cell granulomatous lesions, with no AFB or necrosis, which was suggestive of BCG adenitis.
The BCG vaccine is one of the oldest vaccines used in humans, which has been used for the past 80 years and is one of the most widely used vaccines. Globally, approxi- mately 80% of the infants from developing nations have been covered under national immunization programs. This vaccine has shown a protective effect against disseminated, extrapulmonary, and meningeal TB in children. BCG does not provide protection against primary TB, latent pulmonary infection, and reactivation3.
Under normal circumstances, after vaccination, intradermally over the left deltoid, the BCG starts to spread or disseminate to various parts of the body, including the regional lymph nodes, causing asymptomatic lymphadenopathy. This lymph node enlargement has no clinical significance and resolves on its own over several weeks4. After BCG vaccination, the first reaction is an induration at the injection site, followed by ulceration and crust formation, which often settles down by 6~8 weeks, leaving a scar at the vaccination site; hence, an axillary lymph node enlargement <1 cm can be a normal response following vaccination5.
The diagnosis of BCG lymphadenitis is clinical. A few diagnostic markers include the following:
1. An ipsilateral swelling in the vaccinated site and absence of other medical cause for lymphadenitis6.
2. Absence of fever, tenderness, and other constitutional symptoms differentiating it from pyogenic adenitis.
3. Matted and enlarged discrete lymph nodes, which cannot be differentiated from tubercular lymphadenitis in histo- pathology studies.
Lymphadenitis is a side effect of BCG vaccination in neonates, which may be either related to the host or vaccine6. Other vaccine-related factors are as follows:
a) Vaccine strain used
b) Vaccination technique
c) Vaccine dose
d) Immune status of the child and its physique
Axillary lymph node enlargement was seen in 75% the vaccinees on the ipsilateral side (unilaterally), and this is con- sistent with the presented case8.
Teo et al. reported an increase in BCG-related lymphadenitis after the use of the Danish strain (SSI) type8. This correlates with the current case because the same strain of vaccine was used in our patient. Complications range from mild to disseminated BCG infections, between regional lymphadenitis to suppurative lymphadenitis, osteomyelitis, and disseminated BCG infections9.
In the current case, such disseminated infections after BCG vaccination are rare, and isolated enlargement of the axillary, cervical, or supraclavicular lymph nodes remains the most common complication of BCG vaccination10.
Cartridge-based nucleic acid amplification test (CBNAAT) was positive in our patient, and the results align with the findings of Mandal et al., where two cases were positive in the CBNAAT and had no other signs of TB as in the present study7. In the present study, we used GeneXpert MTB/RIF (Cepheid) test, which detects MTB complex (including MTB and BCG) and its resistance to rifampicin11. This should be kept in mind in cases of post-BCG vaccination lymphadenitis, when a GeneXpert test is performed on the lymph node sample and a positive result is obtained.
The study by Singh10 suggested a higher incidence of nonsuppurative lymphadenitis after BCG vaccination than the suppurative type, and it is often self-limiting and resolves over a period. This condition is often subclinical and is often unnoticed. In this patient, although complications did not arise, the lymph node was excised at the request of the parents. A study conducted in Saudi Arabia12 showed that the most effective treatment for lymph node enlargement caused by BCG injection was medical treatment in addition to needle aspiration, which was not in accordance with our current case where surgical intervention was performed, as per the parents' request.
To our knowledge and review of the available literature, we did not find cases with clinical manifestations similar to this case that were eventually diagnosed as conditions other than BCG adenitis (e.g., active tuberculosis).
This case report is presented to emphasize that BCG adenitis can occur even after the age of 1 year, and careful clinical history and appropriate investigations, along with the know-ledge that GeneXpert MTB detects MTB complex will aid in the correct diagnosis. Therefore, BCG adenitis can persist beyond the typically expected time, and monitoring the child until around 18 months of age is recommended without specific interventions. We also recommend observing the child until around 2 years of age before initiating specific interventions.
References
1. Okafor CN, Rewane A, Momodu II. Bacillus Calmette Guérin. [Updated 2023 Jul 3]. In: StatPearls [Internet]. Treasure Island (FL): Stat Pearls Publishing; 2024
2. https://www.pediatriconcall.com/articles/pediatric-surgery/ bcg-adenitis/bcg-adenitis introduction#9636
3. https://www.who.int/teams/health-product-policy-and-standards/standards-and-specifications/vaccines-quality/ bcg
4. Sonawane D, Mane S, Bhongade M, Kota K, Ansari B. Suppurative BCG lymphadenitis in an infant. J Med Sci Clin Res 2017;5:17440-17444
Google Scholar
5. Venkataraman A, Yusuff M, Liebeschuetz S, Riddell A, Prendergast AJ. Management and outcome of Bacille Calmette-Guérin vaccine adverse reactions. Vaccine 2015; 33:5470-5474
6. Udgaonkar US, Patil SS, Rekha VB, Shah S. Suppurative supraclavicular Bacille Calmette-Guérin lymphadenitis - A case report, awareness and management options. Indian J Med Microbiol 2015;33:S137-139
Google Scholar
7. Mandal M, Nayak P, Mangal S. Bacillus Calmette-Guérin Adenitis: An intriguing series of four cases. National J Lab Med 2024;13:PS05-PS08
8. Teo SS, Smeulders N, Shingadia DV. BCG vaccine associ- ated suppurative lymphadenitis. Vaccine 2005;23:2676-2679
Google Scholar
9. Chaves_Carballo E, Sanchez GA. Regional lymphadenitis following BCG vaccination (BCGitis). Clinical comments based upon 25 instances among 1295 children vaccinees. Clin Pediatr (Phila) 1972;11:693-697
Google Scholar
10. Singh N, Gupta P. Bacillus Calmette-Guerin lymphadenitis in children: an underdiagnosed entity. Int J Community Med Public Health 2024;11:870-873
11. Mukhida S, Vyawahare CR, Mirza SB, Gandham NR, Khan S, Kannuri S, et al. Role of GeneXpert MTB/RIF assay for the diagnosis of cervical lymph node tuberculosis and rifampicin resistance. Tzu Chi Med J 2022;34:418-422
Google Scholar
12. Bukhari E, Alzahrani M, Alsubaie S, Alrabiaah A, Alzamil F. Bacillus Calmette-Guérin lymphadenitis: A 6-year experi- ence in two Saudi hospitals. Indian J Pathol Microbiol 2012;55:202-205
Google Scholar
Congratulatory MessageClick here!