pISSN : 3058-423X eISSN: 3058-4302
Open Access, Peer-reviewed

pISSN : 3058-423X eISSN: 3058-4302
Open Access, Peer-reviewed
Diah Ngesti Kumalasari,Made Putri Hendaria,Arifiana Wungu Kartika Dewi,Maylita Sari,Regitta Indira,Bagus Haryo Kusumaputra,Medhi Denisa Alinda,M.Yulianto Listiawan,Cita Rosita S.Prakoeswa
10.17966/JMI.2024.29.3.165 Epub 2024 October 11
Abstract
Mycobacterium lepromatosis is the primary cause of diffuse lepromatous leprosy and has previously been linked to the Lucio phenomenon in Mexico. In this study, we demonstrate that M. leprae and M. lepromatosis are responsible for many of the leprosy infections in which the Lucio phenomenon occurs. A 47-year-old female presented with chief complaints of erythematous and purpuric lesions on her left lower extremity and bilateral upper extremities. Over the past month, she had experienced recurrent tingling sensations in both legs. The patient had widespread infiltration, no nodules, madarosis (eyelash loss), and thickening in both ears. An acid-fast bacilli analysis revealed a bacterial index of 4+ and a microscopy index of 7%. Biopsy tissue was lacking the epidermal layer, and there was a dermal layer of dilated blood vessels, an area of bleeding, and infiltration of neutrophil inflammatory cells, perivascular plasma cells, foam cells, histiocytes, lymphocytes, the endothelium, and perivascular regions by acid-fast bacilli. A polymerase chain reaction identified the presence of both M. leprae and M. lepromatosis. The patient's symptoms worsened rapidly and she developed ulcers on both hands and both legs, extending to the soles of the feet. She was admitted to the hospital 3 days after presentation. Based on the clinical symptoms, examination of tissue samples, and the polymerase chain reaction identification of coinfection with M. leprae and M. lepromatosis, a diagnosis of diffuse lepromatous leprosy was made. The M. leprae bacteria were verified by DNA sequencing.
Keywords
Diffuse lepromatous leprosy Lucio phenomenon M. leprae M. lepromatosis Tropical disease
Leprosy is caused by the obligate intracellular bacterium Mycobacterium leprae, which manifests as a chronic granulomatous bacterial infection. Indonesia has the third greatest prevalence of leprosy worldwide, after India and Brazil1. Thus, the disease is a significant public health risk, with approxi- mately 15,000 new cases reported each year. However, according to the 2021 Indonesia Health Profile, Indonesia achieved leprosy elimination status in 2000, with a frequency below 1/10,000 people2,3. Leprosy reactions are categorized as type 1, type 2, or type 3. Type 3 is also referred to as the Lucio phenomenon4. In 2008, the bacilli in two instances of leprosy were identified as a new species, which was named M. lepromatosis. An analysis of samples from Mexico and Brazil, and documented instances from other regions of South America uncovered cases in which M. lepromatosis and M. leprae cooccurred. The Lucio phenomenon was most pre- valent in Mexico and Costa Rica5-7. The condition originated in Mexico and spread to multiple nations, including some in Asia6,7. A study was conducted with 120 individuals diag- nosed with leprosy in Mexico. Of the 87 who were positive for the disease on a polymerase chain reaction (PCR) test, 55 (63.2%) patients were found to have M. lepromatosis, 18 (20.7%) had M. leprae, and 14 (16.1%) had both infections. The present case study aims to examine the clinical presen- tation of the Lucio phenomenon, ascertain the optimum diagnostic methods and treatments, and raise awareness of the condition.
A 47-year-old woman presented to the emergency room at Dr. Soetomo Hospital where she was diagnosed with suspected vasculitis and drug-induced eruption. The results of her vascular ultrasound were normal. The patient was referred to the Department of Dermatovenereology and underwent a slit skin smear examination. An acid-fast bacilli (AFB) test yielded a positive result. The patient described the development of ecchymosis and edema on all four limbs over the past 3 days. At first, there was reddish coloration on the legs and both hands. This changed in hue to purple-red and black. She had also experienced a persistent tingling sensation in both legs for the past month, swelling and pain in all four limbs, and enlargement and thickening of both ears. She had received no prior treatment for the complaint. The patient made frequent trips to her brother's residence but was unaware of his leprosy diagnosis some years ago. This was noted in the medical history. The patient's reported travel history did not include regions where the disease is commonly found, specifically Mexico and Central America. However, the patient resides in an area known for the regular occurrence of a particular disease specific to Babat, Lamongan, and East Java.
Upon physical examination, the patient's overall condition was found to be satisfactory. She rated her pain level as 4 on a scale. She had a mild case of anemia. Examination revealed hypoesthesia in the lesions on both legs. A derma- tological assessment of the face identified a condition called madarosis, in which there is loss of the eyebrows and eye- lashes. Additionally, leonine facies was observed. This is a condition caused by a diffuse infiltrate, which is characterized by waxy, shiny, thickened, and enlarged skin. Furthermore, there was enlargement and thickening of both ears. In the antebrachial region, specifically the right and left hands, and the right and left lower leg region, there were various pur- puras with different boundaries. Their sizes ranged from 0.5 × 1 cm to 1 × 1.5 cm and they were covered with blackish crusts, slough, and numerous bullae (Fig. 1). The skin smear examination revealed a bacterial index (BI) of 4+ and a morphological index (MI) of 7% (Fig. 2A) An ELISA anti-phenolic glycolipid I (anti-PGL-1) test showed an immunoglobulin-M (IgM) level of 22.311 μ/mL and an immunoglobulin-G IgG level of 803 μ/mL. Histopathological analysis revealed atrophy of the epidermal and dermal layers and dilated blood vessels. The examination also identified infiltration of neutrophil inflammatory cells, plasma cells, histiocytes, lymphocytes, perivascular cells, and foamy macro- phages. (Fig. 3) Ultimately, it was apparent that the symptoms were compatible with the Lucio phenomena and the lepro- matous leprosy (LL) type of Hansen's disease (Fig. 2). Testing identified two types of bacteria, namely M. leprae and M. lepromatosis (Fig. 2B). Genomic sequencing data confirmed the presence of M. leprae through identification of the nucleotide CTT, which is consistent with M. leprae (Fig. 2C). The patient was diagnosed with diffuse LL caused by M. leprae, with the Lucio phenomenon, anemia, a hemoglobin level of 8.1, a hypoalbuminemia level of 2.97, and prerenal acute kidney injury. The patient was referred to the Nephrology Division of the Internal Medicine Department based on the abnormalities in her laboratory results. Multi-drug therapy was initiated. Dapsone was contraindicated due to the patient's anemia. A daily dose of 40 mg of prednisone was introduced to alleviate the leprosy reaction, with a planned gradual reduction per week. VIP albumin tablets were pre- scribed, to be taken orally three times a day; acid folate tablets, to be taken orally once daily; and one bag of packed red blood cells, by transfusion one a day until her Hb levels were above 10. The patient's fluid balance was maintained.

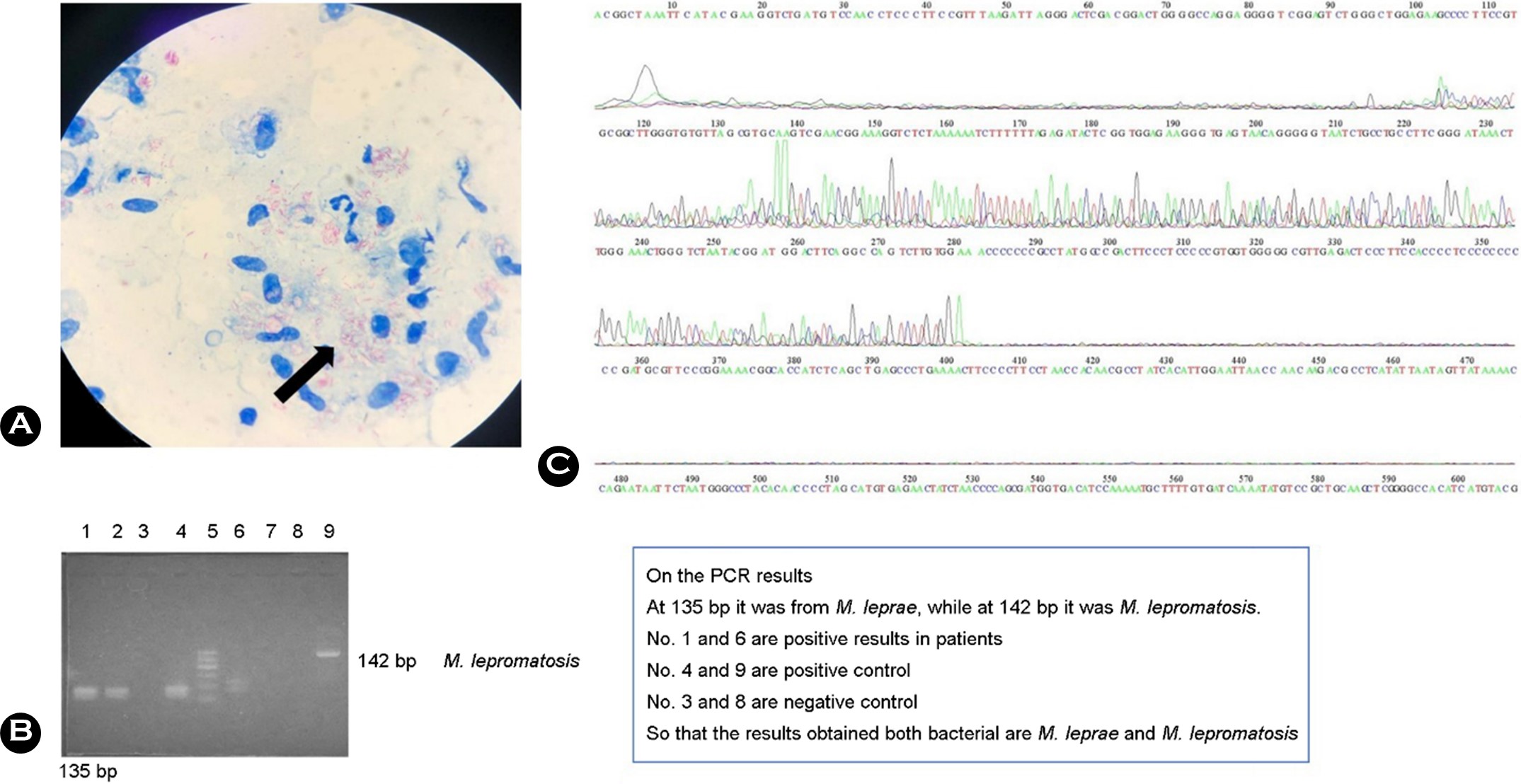
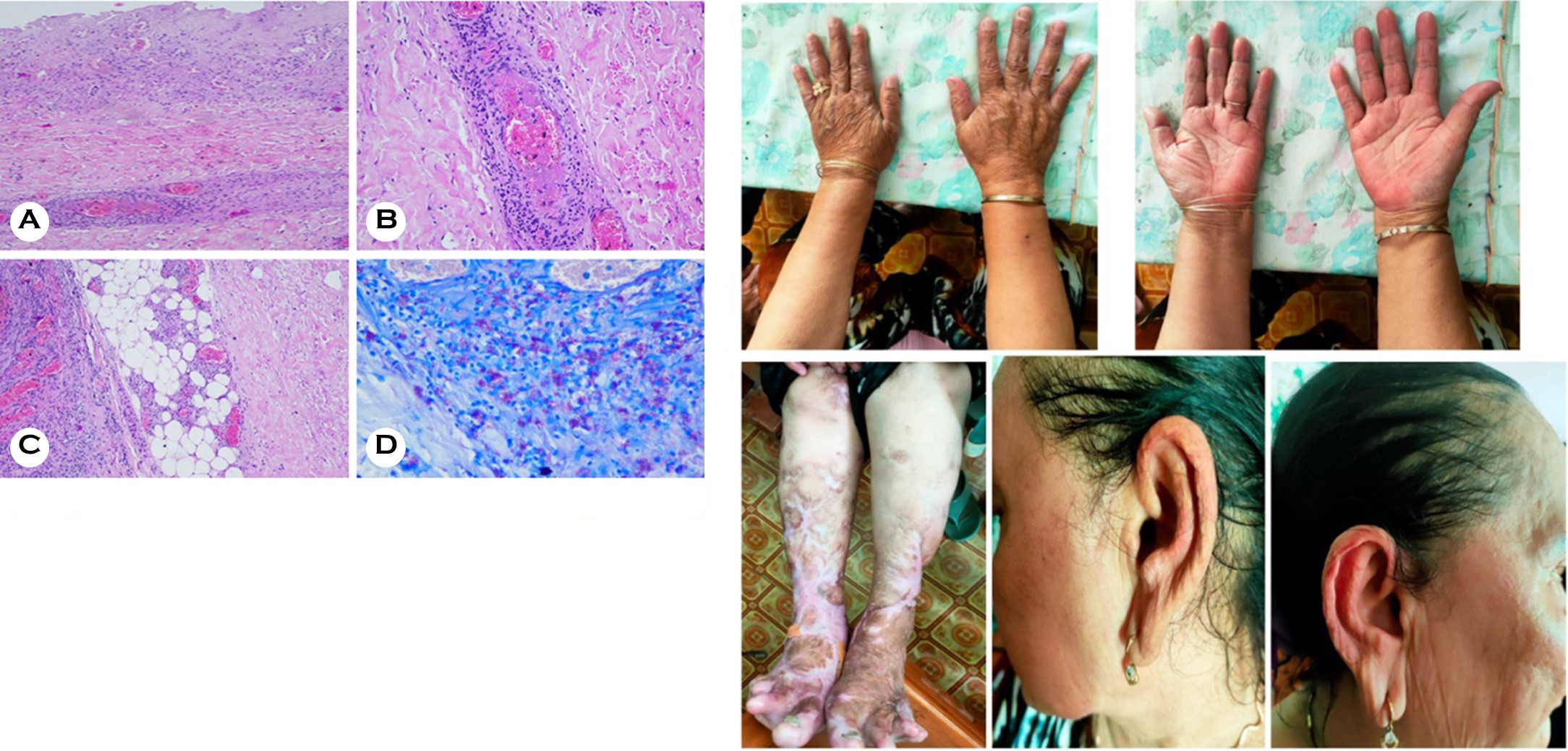
Mycobacterium leprae is the pathogen responsible for the persistent granulomatous disease, leprosy8. Diffuse leproma- tous leprosy (DLL), a variant of LL, is characterized by broad, pervasive infiltration of the skin. The Lucio phenomenon is a type of leprosy reaction known as erythema nodosum leprosum. It is influenced by immune complexes; humoral immunity in particular. The mechanism behind the Lucio phenomenon remains uncertain. However, it is believed to be associated with a significant increase in bacilli replication, leading to widespread skin infiltration. Interleukin-4 (IL-4), interleukin-5 (IL-5), and interleukin-10 (IL-10) cytokines can impede macrophage activation against Mycobacterium and stimulate the production of antibodies. Clinically, a broad infiltration of the skin, resembling myxedema, manifests as a healthy face with thickening of the earlobes. As the illness progresses, edema develops in the hands and legs, causing swelling, puffiness, and redness. It is sometimes referred to as lepra Bonita, which means "pretty leprosy" in Spanish, due to the shiny, myxedema-like appearance of the affected person's skin. In the case described herein, a 47-year-old woman presented with sores and ulcers on her hands and lower limbs, which steadily progressed to painful purpuric lesions and ulcers. This patient was previously untreated for Hansen's disease. The involvement of the face and earlobes indicated diffuse invasion. The patient reported a loss of sensation in a pattern resembling gloves and stockings. There were no light-colored patches on the skin and no neural swelling. During the physical examination, the purpura was described by the patient as a presence that could not be felt. Skin smears produced a BI result of 4+ and an MI value of 7%. Histopathological analysis of the DLL revealed significant infiltration of foamy macrophages in the dermis. These macro- phages contained many AFB (globi), which were inside the cells or the surrounding stroma, lymphocytes, and adnexal structures such as erector muscles. Venules are the pre- dominant location of the vasculitis involved in this type of skin reaction. During the advanced phase, there is a distinct increase in the growth of endothelial cells and the occlusion of blood vessels9. Vessel wall thickening is accompanied by obliteration and thrombosis, necrosis of both the epidermis and dermis, and histiocytic and neutrophilic infiltrates around the nerve fibers, blood vessels, and adnexa4. Patients have atrophy of the epidermis and dermis and noticeable dilation of the blood vessels. There is infiltration of neutrophil in- flammatory cells, plasma cells, histiocytes, lymphocytes, and perivascular and foamy macrophages. A new pathogen called M. lepromatosis was discovered in two Mexican patients who died from DLL5. A PCR test of the patient in this study was positive for M. leprae and M. lepromatosis, indicating a dual infection. The multiple instances of the Lucio phe- nomenon that have been documented in Indonesia have been characterized by dual infection with M. leprae and M. lepromatosis10,11. The process leading to the cooccurrence of these two strains remains unclear. Interestingly, M. leproma- tosis is predominantly found in DLL. A study of DLL patients detected M. lepromatosis in 63.2% and M. leprae in 20.7%. Dual infection with both M. lepromatosis and M. leprae accounted for 16.1% of all instances in which the species were verified.
PCR analysis revealed both M. leprae and M. lepromatosis in our patient, with the presence of M. leprae confirmed by DNA sequencing. The patient was diagnosed with the Lucio phenomenon caused by M. leprae. She received 12 months of treatment for multibacillary leprosy. Wound care involve debridement, which was performed using normal saline solution (0.9%); the application of dressings, which were periodically assessed; and topical antibiotics. It is worth noting that a few fatal cases of this condition have been reported, with sepsis being the primary cause of death.
Lucio phenomenon is an uncommon symptom of leprosy that poses significant diagnostic difficulties. The phenomenon is rarely seen outside of endemic regions, making it challen- ging to identify. Patients with the Lucio phenomenon have mortality risks associated with complications such as severe ulceration, disseminated intravascular coagulation, and sepsis. Early diagnosis and initiation of appropriate treatment greatly improve a patient's prognosis and, in the longer term, their quality of life.
References
1. Indonesia Ministry of Health. Peraturan menteri kesehatan republik Indonesia nomor 11 tahun 2019 tentang penanggulangan kusta. 1st ed. Jakarta: Kementerian Kesehatan RI, 2019
2. Indonesia Ministry of Health. Pedoman Nasional Program Pengendalian Penyakit Lepra. 2012;1-56
3. Indonesia Ministry of Health. Indonesia Health Profile 2018. Jakarta: Kementerian Kesehatan Republik Indonesia, 2019
4. Kumar B, Dogra S. Case definition and clinical types of leprosy. In: Kumar B, Kar K (eds) IAL Textbook of leprosy. New Delhi: Jaypee Brothers Medical Publishers, 2017, pp. 236-253
5. Han XY, Aung FM, Choon SE, Werner B. Analysis of the leprosy agents Mycobacterium leprae and Mycobacterium lepromatosis in four countries. Am J Clin Pathol 2014; 142:524-532
Google Scholar
6. Velarde-Félix JS, Alvarado-Villa G, Vera-Cabrera L.
Google Scholar
7. Curi PF, Villaroel JS, Migliore N, Albertengo A, Aquino ML, Ceccato F, et al. Lucio's phenomenon: report of five cases. Clin Rheumatol 2016;35:1397-1401
Google Scholar
8. Fischer M. Leprosy – an overview of clinical features, diagnosis, and treatment. J Dtsch Dermatol Ges 2017;15: 801-827
Google Scholar
9. Sehgal VN. Lucio's phenomenon/erythema necroticans. Int J Dermatol 2005;44:602-605
Google Scholar
10. Prakoeswa CRS, Herwanto N, Agusni RI, Natalya FR, Listiawan MY, Adriaty D. Lucio phenomenon of leprosy LL type on pregnancy: A Rare Case. Lepr Rev 2016;87: 526-531
Google Scholar
11. Adriaty D, Karim A, Putra BH, Agusni RI, Wahyuningtyas PA, Wahyuni R, et al. Analysis Mycobacterium leproma-tosis as the causative agent of diffuse lepromatous leprosy patient in Indonesia. Biodiversitas 2023;24:4521-4529
Google Scholar
Congratulatory MessageClick here!