pISSN : 3058-423X eISSN: 3058-4302
Open Access, Peer-reviewed

pISSN : 3058-423X eISSN: 3058-4302
Open Access, Peer-reviewed
Hoon Choi,Jun Ho Kwak,In Ho Bae,Bong Seok Shin,Min Sung Kim,Chan-Ho Na
10.17966/JMI.2024.29.2.78 Epub 2024 July 07
Abstract
Chromoblastomycosis, a chronic cutaneous mycosis caused by pigmented fungi, is typically associated with trauma in the exposed parts of the body. We report a 68-year-old male farmer diagnosed with chromoblastomycosis clinically mimicking a cutaneous abscess on the back, an unusual location. Histopathological and mycological examination identified Fonsecaea pedrosoi. Treatment with itraconazole and cryotherapy showed improvement after 4 months. High suspicion index and biopsy are imperative for early diagnosis of chromoblastomycosis. This case adds to the limited cases reported in Korea, emphasizing the importance of considering chromoblastomycosis in diverse clinical presentations.
Keywords
Chromoblastomycosis Fonsecaea pedrosoi Fungus
Chromoblastomycosis is a chronic and progressive granu-lomatous cutaneous mycosis caused by pigmented fungi. Fungal inoculation typically occurs at the site of traumatic skin injury with lesions manifesting weeks to months after trauma. The infection commonly occurs in the exposed parts of the body, such as the lower and upper limbs1-3. Clinical pre- sentation includes the development of nodules and verrucous plaques that eventually undergo ulceration4. Chromoblasto- mycosis is most prevalent in tropical and subtropical regions, but only a few cases have been reported in Korea5,6. We report a 68-year-old man with chromoblastomycosis, notable for its occurrence in an unusual area, such as the back, with skin lesions resembling a cutaneous abscess.
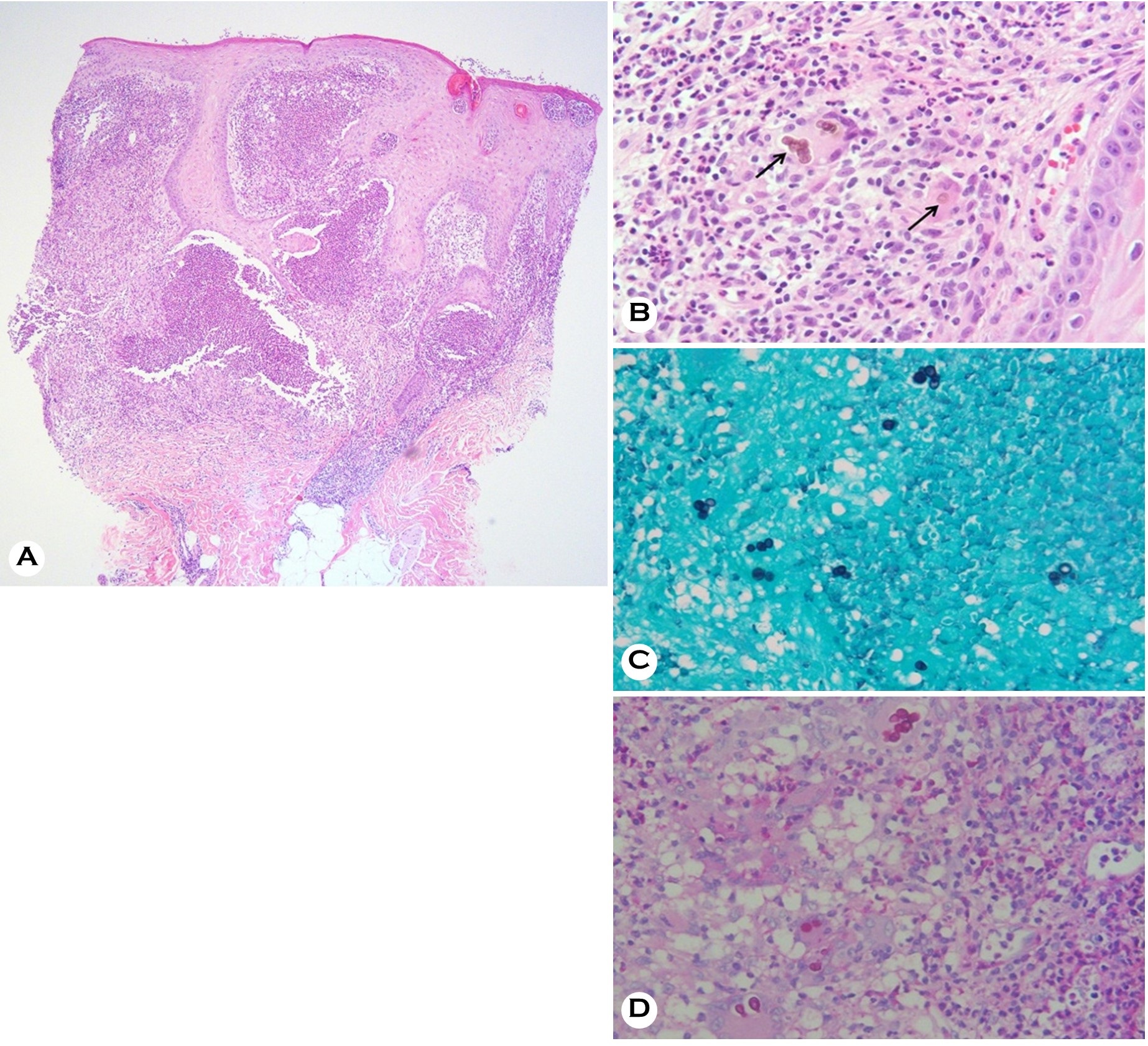
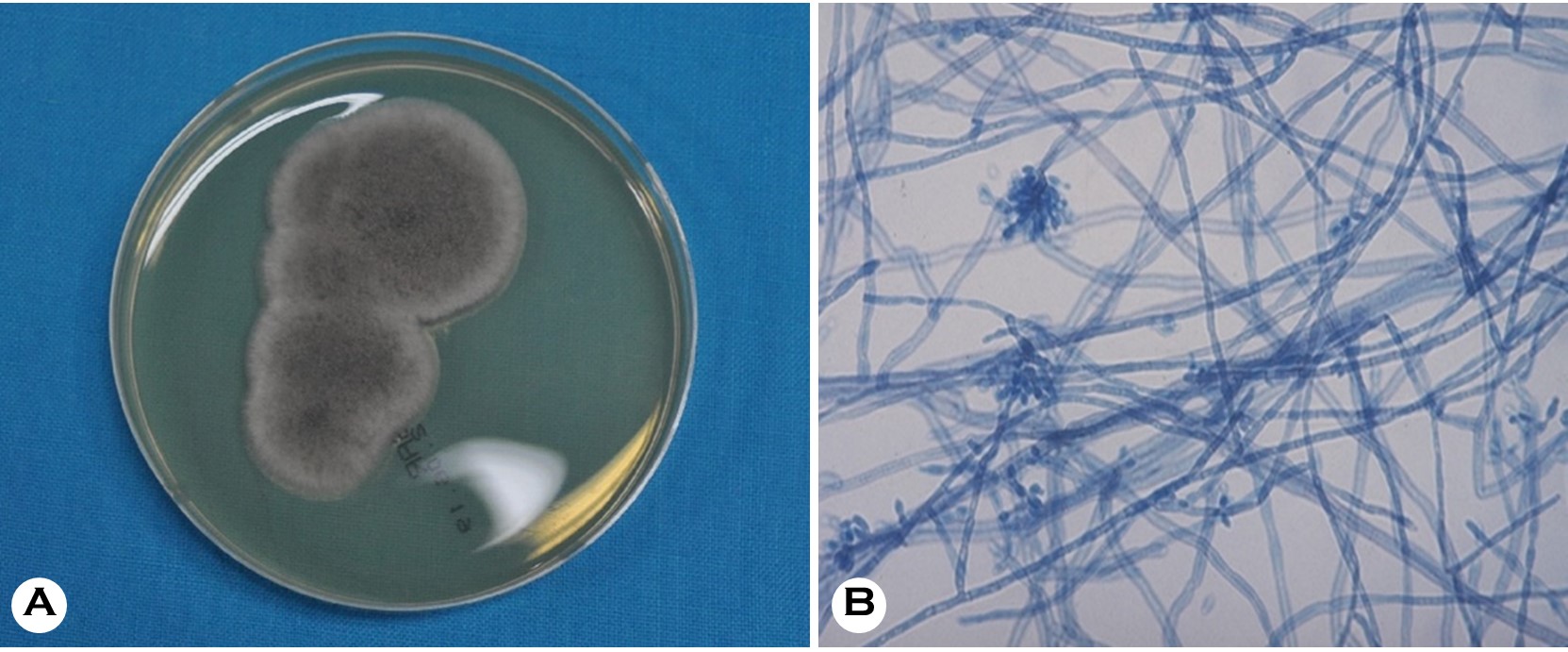
A 68-year-old male farmer presented with two asymp- tomatic erythematous nodules on the left part of the upper back that had been present for 7 months (Fig. 1). His past medical history was unremarkable and there was no history of trauma. He was earlier diagnosed as a case of cutaneous abscess at another clinic and underwent incision and drain- age with empirical antibiotic therapy. However, the lesions continued to persist. Consequently, a punch biopsy was performed to rule out infectious disease. Histopathological examination revealed hyperkeratosis, parakeratosis, marked acanthosis, pseudoepitheliomatous epidermal hyperplasia, and intraepidermal microabscesses in the epidermis. A lichen- oid granulomatous inflammatory pattern was observed in the dermis with the presence of neutrophilic microabscesses in the granulomatous area (Fig. 2A). Additionally, there were prominent, golden-brown thick-walled, ovoid spores, resembling "copper pennies" (Fig. 2B). The presence of fungi was confirmed by Grocott's methenamine silver (GMS) and Periodic acid-Schiff (PAS) staining (Fig. 2 C and D). Two weeks later, colonies were observed on Sabouraud's dextrose agar (SDA) at room temperature. The colonies were dark green, and the reverse view was black. Microscopic examination of colonies cultured in SDA and stained with lactophenol-cotton blue revealed erect, septate, and sympodial conidiophores. The distal ends of the conidiophores were slightly swollen to form single-celled conidia, that became branched (Fig. 3 A and B). Fonsecaea pedrosoi was identified based on the typical histomorphological characteristics and fungal culture. Following the diagnosis of chromoblastomycosis due to F. pedrosoi, the patient was prescribed itraconazole 200 mg daily, topical isoconazole, and cryotherapy with liquid nitrogen. After 4 months of treatment, the lesions showed improvement.

Chromoblastomycosis is a chronic cutaneous and sub- cutaneous fungal infection primarily caused by melanized fungi. These fungi are characterized by their brown pigmen- tation due to the production of melanin. The fungi often reside in the soil, wood, and plants. Chromoblastomycosis occurs worldwide, but is more prevalent in tropical and temperate regions, predominantly affecting individuals with occupational exposure to the fungi in the environment6. At least 41 species of fungi have been reported to cause chromo- blastomycosis5. In Korea, a few types such as F. monophora, F. pedrosoi, Phialophora richardsiae, Phialophora verrucosa, and Rhinocladiella aquaspersa, have been reported, and the number of cases reported in the literature is small compared to other countries5-8.
Chromoblastomycosis is indeed considered an occupational disease, particularly prevalent among agricultural workers1. The infection is attributed to the invasion of the skin by the fungus at the site of trauma, leading to the development of skin lesions. These lesions typically occur in the exposed areas that are unprotected by clothing. The arms, and especially the lower extremities are the most commonly involved sites in cases of chromoblastomycosis1-3. However, not all patients may recall a specific history of trauma at the site of the lesion7. This may be attributed to a prolonged latency period9.
The lesions can manifest in various forms, including nodular, tumorous, verrucous, cicatricial, and plaque lesions4. The diverse nature of these skin lesions may pose a diagnostic challenge. Thus, histological and mycologic examinations are imperative to identify the fungal infection. The typical histo- logical characteristics of chromoblastomycosis are pseudo- epitheliomatous epidermal hyperplasia, intraepidermal micro- abscesses, and mixed granuloma. Dark brown, ovoid, or spherical spores resembling "copper pennies" indicate mela- nized fungi as the causative pathogen. This appearance can be easily visualized by Hematoxylin and Eosin staining. Additionally, special stains such as GMS and PAS can help support the diagnosis by highlighting the fungal elements10. These histopathological features are crucial for distinguishing chromoblastomycosis from other skin conditions.
Initial identification of putative species in chromoblasto- mycosis is often performed using mycological and morpho- logical methods. The species of Fonsecaea display erect, septate, and sympodial conidiophores that are extensively branched at their apices. Phialophora verrucosa has a mono- morphic morphology characterized by flask-shaped phialides. Rhinocladiella aquaspersa features erect, brown, septate conidiophores, bearing conidia at their terminal parts11. These traditional methods of examining morphological characteristics are time-consuming. However, the advances in diagnostic technology have enabled rapid identification of the fungal species. Molecular techniques, such as gene sequencing analysis are used for the definitive identification of fungal species12,13. A limitation of this study is that molecular analysis for identifying the causative fungus was not performed. The morphological characteristics observed in this case were consistent with Fonsecaea species. Although F. monophora and F. pedrosoi are morphologically very similar, F. pedrosoi was identified as the causative agent in this case based on the fact that F. pedrosoi generally has slightly shorter conidial chains and slightly longer denticles than F. monophora12.
To the best of our knowledge, 10 cases of chromoblasto- mycosis have been reported in Korea (Table 1). In these cases, the lesions predominantly manifested in the exposed parts of the body, exhibiting diverse clinical presentations. Our patient presented with a nodule resembling a cutaneous abscess, obscuring the diagnosis. Notably, only two previous cases with lesions in the non-exposed areas (abdomen and breast) have been reported in Korea8,14. This case represents the first instance of chromoblastomycosis caused by F. pedrosoi in non-exposed areas. Despite the denial of any history of trauma, the possibility of chromoblastomycosis was consid- ered, especially given his occupation as a farmer.
|
Case |
Reference |
Sex |
Age |
Location |
Lesion |
Causative |
Diagnostics for |
Treatment |
|
1 |
Suh et al. |
M |
58 |
Wrist |
Plaque |
Fonsecaea |
Fungal culture, |
ILI APB |
|
2 |
Kim et al. |
M |
68 |
Hand |
Verrucous |
Fonsecaea |
Fungal culture, |
Oral ICZ |
|
3 |
Kim et al. |
F |
65 |
Arm |
Annular |
Fonsecaea |
Fungal culture, |
Topical APB |
|
4 |
Kang et al. |
F |
56 |
Hands |
Erythematous |
Fonsecaea |
Fungal culture, |
Oral ICZ, surgical |
|
5 |
Lee et al. |
M |
54 |
Leg |
Plaque |
Fonsecaea |
Fungal culture, |
Oral terbinafine |
|
6 |
Jun et al. |
F |
52 |
Abdomen |
Erythematous |
Rhinocladiella |
Fungal culture, |
Oral ICZ, surgical |
|
7 |
Park et al. |
F |
37 |
Breast |
Verrucous plaques |
Phialophora |
Fungal culture, |
IV APB, oral |
|
8 |
Son et al. |
M |
43 |
Leg |
Verrucous plaque |
Phialophora |
Fungal culture, microscopy, |
Oral ICZ, |
|
9 |
Kim et al. |
F |
61 |
Forearm |
Erythematous |
Fonsecaea |
Fungal culture, microscopy, |
Local heat therapy, |
|
10 |
Lee et al. |
M |
65 |
Forearm |
Erythematous |
Fonsecaea |
Molecular analysis |
Oral ICZ |
|
Present |
Choi et al. |
M |
68 |
Back |
Erythematous |
Fonsecaea |
Fungal culture, |
Cryotherapy, oral ICZ,
topical isoconazole |
|
APB, amphotericin B; ICZ, itraconazole; ILI,
intralesional injection; IV, intravenous |
||||||||
In conclusion, we suggest that the possibility of chromo- blastomycosis should be considered in individuals presenting with skin lesions, especially those with an occupational back- ground as farmers. Early recognition and diagnosis are pivotal for effective management, and conducting a biopsy, as exemplified in this case, is a crucial step for accurate diagnosis. The authors report this rare and interesting case along with a review of pertinent literature.
References
1. Verma S, Thakur BK, Raphael V, Thappa DM. Epidemi- ology of subcutaneous mycoses in northeast India: A retrospective study. Indian J Dermatol 2018;63:496-501
Google Scholar
2. Minotto R, Bernardi CD, Mallmann LF, Edelweiss MI, Scroferneker ML. Chromoblastomycosis: a review of 100 cases in the state of Rio Grande do Sul, Brazil. J Am Acad Dermatol 2001;44:585-592
Google Scholar
3. Correia RT, Valente N, Criado PR, Martins JE. Chromo- blastomycosis: study of 27 cases and review of medical literature. An Bras Dermatol 2010;85:448-454
Google Scholar
4. Queiroz-Telles F, Esterre P, Perez-Blanco M, Vitale RG, Salgado CG, Bonifaz A. Chromoblastomycosis: an over- view of clinical manifestations, diagnosis and treatment. Medical Mycology 2009;47:3-15
Google Scholar
5. Passero LFD, Cavallone IN, Belda W Jr. Reviewing the Etiologic Agents, Microbe-Host Relationship, Immune Response, Diagnosis, and Treatment in Chromoblasto- mycosis. J Immunol Res 2021;2021:9742832
Google Scholar
6. Queiroz-Telles F. Chromoblastomycosis: a neglected trop- ical disease. Rev Inst Med Trop Sao Paulo 2015;7(Suppl 19):46-50
Google Scholar
7. Son YM, Kang HK, Na SY, Lee HY, Baek JO, Lee JR, et al. Chromoblastomycosis caused by Phialophora richardsiae. Ann Dermatol 2010;22:362-366
Google Scholar
8. Jun JB, Park JY, Kim DW, Suh SB. Chromoblastomycosis Caused by Rhinocladiella aquaspersa. Korean J Med Mycol 2004;9:117-122
Google Scholar
9. Brandt ME, Warnock DW. Epidemiology, clinical manifest- ations, and therapy of infections caused by dematiaceous fungi. J Chemother 2003;15(Suppl 2):36-47
Google Scholar
10. Elder D, Elenitsas R, Murphy GF, Rosenbach M, Rubin AI, Seykora JT, et al. Fungal diseases. In: Hinshaw MA, Longley B.J, editors. Lever's dermatopathology: histopathology of the skin. 12th ed. Singapore: Wolters Kluwer, 2022: 729
Google Scholar
11. Queiroz-Telles F, de Hoog S, Santos DW, Salgado CG, Vicente VA, Bonifaz A, et al. Chromoblastomycosis. Clin Microbiol Rev 2017;30:233-276
Google Scholar
12. De Hoog GS, Attili-Angelis D, Vicente VA, Van Den Ende AH, Queiroz-Telles F. Molecular ecology and pathogenic potential of Fonsecaea species. Med Mycol 2004;42: 405-416
Google Scholar
13. Lee WJ, Eun DH, Park JH, Jang YH, Lee SJ, KIM DW, et al. A case of Fonsecaea monophora infection. Korean J Med Mycol 2017;22:141-143
Google Scholar
14. Park SG, Oh SH, Suh SB, Lee KH, Chung KY. A case of chromoblastomycosis with an unusual clinical manifest- ation caused by Phialophora verrucosa on an unexposed area: treatment with a combination of amphotericin B and 5-flucytosine. Br J Dermatol 2005;152:560-564
Google Scholar
15. Suh MK, Sung YO, Yoon KS, Ha GY, Kim JR. A case of chromoblastomycosis caused by Fonsecaea pedrosoi. Korea J Dermatol 1996;34:832-836
Google Scholar
16. Kim HU, Son GY, Ihm CW. A case of chromoblasto- mycosis showing a good response to itraconazole. Ann Dermatol 1997;9:51-54
Google Scholar
17. Kim SW, Oh SH, Choi SK, Lee YH, Yoon JH, Bang YJ, et al. Chromoblastomycosis treated with occlusive dressing of amphotericin B cream. Korean J Med Mycol 2000;5:144-149
Google Scholar
18. Kang NG, Suh MK, Park SG, Song KY, Kim TH. A case of chromomycosis showing ulcerative lesions on dorsa of hands. Korea J Dermatol 2002;40:174-176
Google Scholar
19. Lee CW, Sim SJ, Song KH, Kim KH. A case of chromo- blastomycosis treated with terbinafine. Korean J Med Mycol 2003;8:26-29
Google Scholar
20. Kim BS, Choi JH, Sohng SH, Shin DH, Choi JS, Suh MK. Chromoblastomycosis caused by Fonsecaea monophora. Korean J Med Mycol 2014;19:18-24
Google Scholar
Congratulatory MessageClick here!