pISSN : 3058-423X eISSN: 3058-4302
Open Access, Peer-reviewed

pISSN : 3058-423X eISSN: 3058-4302
Open Access, Peer-reviewed
Karine Annisa Prakasita,Dwi Murtiastutik,Alfina Multaza Rahmi,Diah Ngesti Kumalasari
10.17966/JMI.2024.29.1.15 Epub 2024 March 28
Abstract
Pediculosis capitis, commonly known as head lice infestation, is caused by head lice, a type of ectoparasite that affects the human scalp. Excessive scratching of the scalp due to itching can lead to skin damage and bacterial infection. In severe cases of infestation, it can cause iron deficiency anemia. This case report presents a 29-year-old female with pediculosis capitis and secondary infection. The patient had a low hemoglobin level of 7.8 g/dL, indicating anemia despite no history of bleeding. The patient was successfully treated with permethrin 1% lotion, antibiotics, ferrous sulfate, and folic acid. Proper treatment of pediculosis capitis, including its complications, and educating the patients are equally essential to combat the infestation and prevent the spread of the parasites.
Keywords
Anemia Pediculosis capitis Secondary infection
Pediculosis capitis is an ectoparasitic infestation of the human scalp caused by head lice. The condition is also known as pediculosis humanus capitis1. A head lice infestation can affect anyone, particularly those residing in rural and developing areas. Although pediculosis capitis is not a major health problem, it may cause skin irritation, secondary in- fections, embarrassment, isolation, criticism from others, and psychological distress2,3.
Severe head lice infestations are inadequately reported in the literature. Repeated scalp scratching due to pruritus can compromise the skin's integrity, potentially leading to sec- ondary bacterial infections or impetigo3. An untreated, severe head lice infestation coupled with a dietary iron deficiency may increase the risk of anemia4. This situation, known as hyperinfestation, can cause iron deficiency anemia because the lice survive off blood taken from their host. Although very little blood is ingested during a single feeding, an individual with a severe head lice infestation may, over an extended period, become more susceptible to iron deficiency anemia5.
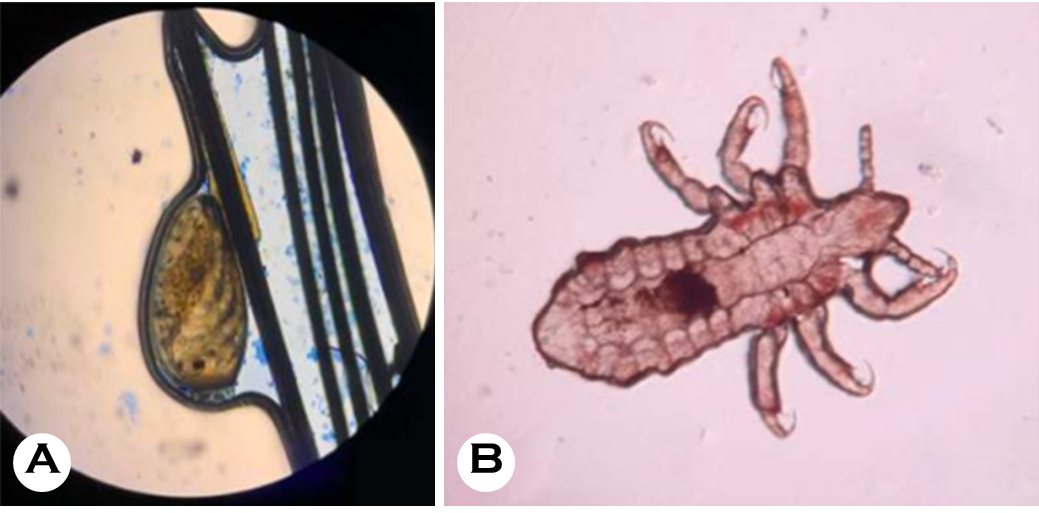
A 29-year-old woman presented to an outpatient clinic with a large lump on her head that had been gradually increasing in size for two weeks. Initially, the lump was approximately the size of a marble; however, it quickly in- creased in size. She reportedly experienced pain around the lump. One week before her visit, she developed a purulent wound on top of the lump. She was febrile three days before her visit and reported a four-month period where she experienced itching. Lice and nits were visible on her scalp. The patient reported bathing once daily, but rarely washed her hair. Her past medical history was significant for depression and she had been taking antidepressants regularly for a year. She spent most of her time inside her house and slept in a bed. The patient's mother and sister, both of whom regularly used the patient's comb, also reported scalp itching and lice. The patient's other symptoms included generalized fatigue and light-headedness. During the physical examination, the patient appeared tired; however, her vital signs were stable. The examination revealed pale conjunctiva, indicative of anemia. A close examination of her scalp revealed a 10-cm red nodule that was tender and warm to the touch and visible purulent. Other examination findings included alopecia, multiple lice, and multiple nits on her hair strands (Fig. 1). A scraping examination revealed nits attached to a hair shaft and an adult louse (Fig. 2). Gram staining examination of the pus showed gram-positive bacteria (Fig. 3).

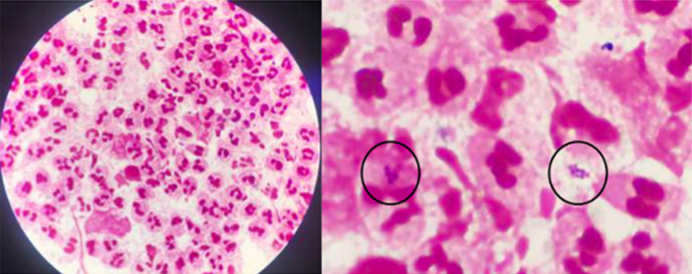
The patient's blood test results showed a hemoglobin level of 7.8 g/dL (N: 11.5~13.5 g/dL), slightly increased leukocytes of 11.79 × 103/μL (N: 4.0~11.0 × 103/μL), a serum iron level of 30 μg/dL (N: 60~170 μg/dL), a total iron binding capacity of 478 μg/dL (N: 240~450 μg/dL), and a ferritin level of 43.8 ng/mL (N: 10~120 ng/mL). A blood smear examination revealed microcytic hypochromic anemia. The final diagnosis—based on the patient's history, physical exam- ination, and laboratory tests—was pediculosis capitis with a secondary infection and iron deficiency anemia.
The patient was treated with 1% permethrin lotion, applied topically to the scalp and hair and left for 10 minutes before rinsing. This process was repeated after 7 days. For the sec- ondary infection, the patient was prescribed erythromycin (500 mg) to be taken four times daily for 7 days and acet- aminophen (500 mg) to be taken up to three times daily when experiencing fever or lesion pain. The lesion was treated with a 0.9% NaCl wet dressing twice daily for 10~15 minutes, followed by application of 2% fucidic acid cream. She was referred to internal medicine to treat her anemia and pre- scribed a ferrous sulfate tablet (200 mg) to be taken three times daily and folic acid (1 mg) to be taken three times daily. She was additionally advised to increase her protein and iron consumption, avoid sharing combs and towels with other people, maintain scalp hygiene by washing her hair daily, and avoid touching the lesion. After 2 weeks of treatment, no lice and nits were found on her scalp, and the nodule appeared to have decreased in size (Fig. 4). After the treatment, the patient's hemoglobin levels also slightly increased to 9.5 g/dL.

Infestation of Pediculus humanus capitis, which causes pediculosis capitis, is a major public health concern. These parasitic insects require a living host to survive and as a source of blood. According to a study6, an adult female louse feeds three to five times daily and can consume up to 0.0001579 mL of blood in a single feed. Therefore, a severe lice infestation can lead to a loss of about 0.7 mL of blood per day or 20.8 mL per month. Such a loss may not be significant in a healthy and well-nourished person experiencing a short-term infestation. However, a persistent infestation can cause significant blood loss, potentially leading to clinically significant anemia. While there is no established link between iron deficiency anemia and lice infestation, both conditions have been reported in children and adults7.
Head lice are predominantly transmitted through direct physical contact, with head-to-head contact being the most common route. Head lice mainly reside on the scalp, with nits often clustered in the occipital and retroauricular regions. Itching is a common symptom caused by sensitivity to louse-related debris in bites or waste. Scratching can damage the skin, lessening skin integrity and setting the stage for a secondary bacterial infection. In severe cases, pyoderma can lead to cicatricial alopecia. Studies indicate that pediculosis capitis is the most common cause of scalp pyodermas in developing countries2. Severe iron deficiency anemia has been linked to heavy and persistent lice infestations. Lice in- festations should be investigated as a potential contributor to iron deficiency anemia in individuals with poor hygiene—including children, unhoused individuals, and patients with psychiatric conditions7. Optimally, lice treatment should priori- tize safety, nontoxicity, over-the-counter accessibility, efficacy, and affordability. In addition, local resistance patterns, user convenience, and cost must be factored into treatment selection8.
Confirmed cases of head lice case are usually treated with topical pesticides and oral medications. External parasite infestations are generally treated by maximizing drug uptake by the parasite while minimizing systemic absorption in the patient2. Head lice treatments seek to eliminate adult lice and their nits safely and effectively. Three reliable treatment options for head lice include topical medications, wet combing, and oral pharmacologic therapy under specific circum- stances. Antistaphylococcal medications can be initiated with patients who exhibit potential bacterial infections. Further microbiological testing is necessary to guide targeted anti- biotic therapies2.
While pediculicide treatments are extremely effective against head lice, challenges such as variable ovicidal activity, the potential for treatment nonadherence, increasing resistance in lice, and risk of reinfestation from contaminated objects necessitate repeated applications of all insecticidal treatments after one week9. Pyrethrins and permethrin are the most commonly used pediculicides; both feature minimal percu- taneous absorption and favorable safety profiles but quickly immobilize and kill lice7.
Preventing head lice hinges on improved detection, management, and treatment to interrupt the transmission cycle. Optimization of environmental and personal hygiene is also important. When someone is diagnosed and treated, their close contacts and household members should also be examined for potential infestations. Environmental disinfection is recommended to prevent reinfestation and thorough elimination1.
In conclusion, effective head lice interventions should include comprehensive education for the public and healthcare professionals, along with clearly defined treatment protocols.
References
1. Bohl B, Evetts J, McClain K, Rosenauer A, Stellitano E. Clinical practice update: pediculosis capitis. Pediatr Nurs 2015;41:227-234
Google Scholar
2. Madke B, Khopkar U. Pediculosis capitis: an update. Indian J Dermatol Venereol Leprol 2012;78:429-438
Google Scholar
3. Durand R, Andriantsoanirina V, Brun S, Laroche L, Izri A. A case of severe pediculosis capitis. Int J Dermatol 2018; 57:e14-15
Google Scholar
4. Nunes C, Moroni R, Mendes J, Justiniano S, Moroni F. Head lice in hair samples from youths, adults, and the elderly in Manaus, Amazonas State, Brazil. Rev Inst Med Trop Sao Paulo 2015;57:239-244
Google Scholar
5. Guss DA, Koenig M, Castillo EM. Severe iron deficiency anemia and lice infestation. J Emerg Med 2011;41:362-365
Google Scholar
6. Al Ghadeer HA, Busaleh F, Albahrani HM, Albisher AM, AlHassan A, AlAmer HM, et al. Pediculosis is a risk factor for iron deficiency anaemia. Cureus 2022;14:e22403
Google Scholar
7. Smith CH, Goldman RD. An incurable itch: Head lice. Can Fam Physician 2012;58:839-841
Google Scholar
8. Devore CD, Schutze GE, Council on School Health and Committee on Infectious Diseases, American Academy of Pediatrics. Head lice. Pediatrics 2015;135:e1355-1365
Google Scholar
9. Wheat CM, Burkhart CN, Burkhart CG, Cohen BA. Scabies, other mites, and pediculosis. In: Kang S, Amagai M, Bruckner AL, Enk AH, Margolis DJ, McMichael AJ, et al., editors. Fitzpatrick's Dermatology 9th Edition. McGraw-Hill; 2019. p. 3274-3286
Google Scholar
Congratulatory MessageClick here!