pISSN : 3058-423X eISSN: 3058-4302
Open Access, Peer-reviewed

pISSN : 3058-423X eISSN: 3058-4302
Open Access, Peer-reviewed
Bogyeong Go,Doyeon Kim,Kyung Eun Jung,Young Lee,Young-Joon Seo,Dongkyun Hong
10.17966/JMI.2023.28.4.113 Epub 2024 January 05
Abstract
Since the emergence of coronavirus disease 2019 (COVID-19), several reports have described various skin manifestations associated with COVID-19. Retiform purpura is a cutaneous manifestation that is likely associated with coagulopathy in patients with severe COVID-19. Here, we present the case of a 62-year-old man with hypertension and multiple myeloma who presented with retiform purpuric patches on both legs two days after a chemotherapy session with carfilzomib and dexamethasone. He had no other respiratory symptoms or fever; however, he was hospitalized for supportive care and underwent COVID-19 screening with reverse transcriptase polymerase chain reaction, which was positive. Histopathologic evaluation of the two punch biopsy samples obtained from the affected skin revealed perivascular lymphocytic lesions with fibrinoid degeneration, extravasated red blood cells, and fibrin deposition in the deep dermis. Based on these findings, the patient was diagnosed with COVID-19 and retiform purpura. He received intensive care after developing fever, cough, sputum production, and dyspnea. However, the patient developed multifocal cerebral infarctions and eventually died. Dermatologists should recognize retiform purpura, which may appear before other COVID-19 symptoms, as an alarm sign which can aid in the prompt implementation of appropriate treatment.
Keywords
Coronavirus disease 2019 Retiform purpura Severe acute respiratory syndrome coronavirus
Coronavirus disease 2019 (COVID-19) is an infectious re- spiratory illness caused by severe acute respiratory syndrome coronavirus 2 and manifests with respiratory symptoms such as cough, shortness of breath, sore throat, and fever. Additionally, various dermatologic manifestations, including morbilliform or pernio-like rash, urticaria, macular erythema, vesicular or papulosquamous lesions, and retiform purpura, have been reported to occur in conjunction with respiratory symptoms in patients with COVID-19. Among these, retiform purpura is a rarely reported manifestation in patients with severe COVID-191. In this report, we present the case of a patient with retiform purpura and COVID-19 who followed a severe disease course, including other thrombotic events and death.
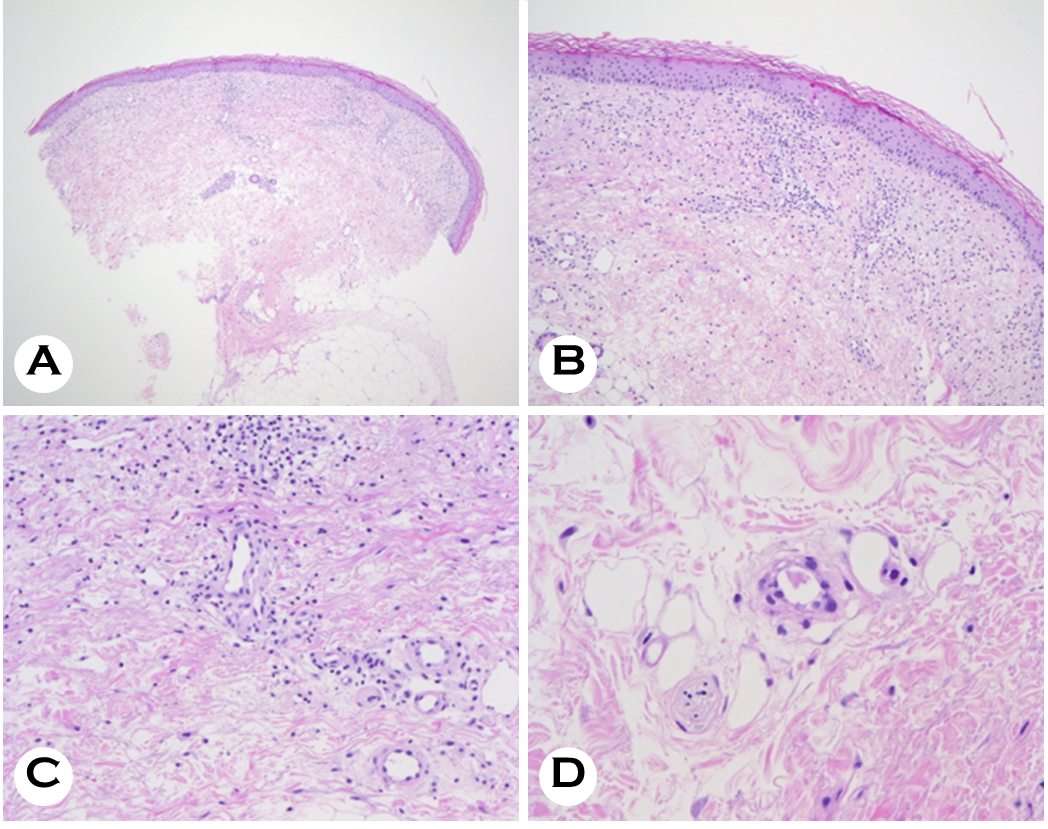
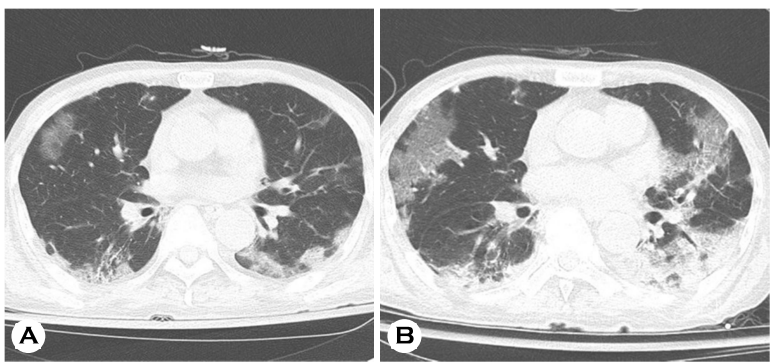
A 62-year-old man presented with asymptomatic retiform purpura and petechiae on both lower limbs that emerged ten days before admission (Fig. 1A-C). He was admitted to the Hematology-Oncology Department for supportive care, and dermatologic consultation was sought to assess the skin lesions. The lesions emerged initially on bilateral calves and gradually spread toward the thighs. These lesions were initially localized to the lower limbs but gradually extended to involve both the upper limbs and trunk. The patient did not report any subjective symptoms related to the skin lesions and denied other systemic symptoms, including fever, cough, sputum, rhinorrhea, and shortness of breath, at the onset of the skin lesions. The patient was previously diagnosed with multiple myeloma and was receiving maintenance therapy with carfilzomib and dexamethasone. The skin lesions de- veloped two days after the eighth chemotherapy cycle, and similar skin lesions were not observed following previous chemotherapy cycles. The patient was also taking amlodipine (5 mg/day) for hypertension and acetylsalicylic acid (100 mg/ day) for atrial fibrillation, with no recent changes or additions to the medications. Routine blood tests prior to the most recent chemotherapy cycle showed a hemoglobin level of 10.7 g/dL, white blood cell count of 3,000/mm3, and platelet count of 49,000/mm3. Subsequent blood tests after the development of skin lesions showed pancytopenia with a hemoglobin level of 7.8 g/dL, white blood cell count of 2,000/mm3, and platelet count of 18,000/mm3. Coagulation tests revealed no abnormalities except for an elevated D-dimer level (388 ng/mL; reference range, 0~243 ng/mL). The patient did not complain of any respiratory symptoms; however, reverse transcriptase polymerase chain reaction for COVID-19 screening according to the hospital infection control guidelines was positive. The patient was referred to the Department of Dermatology for the biopsy of the skin lesions. Histologic examination revealed few necrotic keratino- cytes and basal vacuolar changes in the epidermis (Fig. 2A, B). Perivascular lymphohistiocytic infiltration was observed in the dermis. Although vasculitis was not observed, dilated dermal vessels with endothelial cell swelling and intravascular thrombi were observed (Fig. 2C, D). After admission, the patient was confirmed to have COVID-19 and subsequently developed associated symptoms including fever, cough, and sputum production. Shortness of breath, increased respiratory rate, and decreased oxygen saturation were also observed. Despite appropriate oxygen therapy and supportive care, his oxygen demand continued to increase. Chest radiography and computed tomography revealed COVID-19-related pneu- monia (Fig. 3A) with worsening of the pulmonary findings (Fig. 3B). Acetylsalicylic acid was discontinued due to pro- gressive skin lesions, and the patient gradually developed altered mentality, motor weakness, and dysarthria. Magnetic resonance imaging revealed multiple cerebral infarctions (Fig. 4). The patient eventually died of COVID-19-associated respiratory failure.


COVID-19 primarily manifests with respiratory symptoms; however, several reports suggest an association between COVID-19 and various dermatologic manifestations2,3. Accord- ing to Freeman et al., among the diverse skin lesions asso- ciated with COVID-19, retiform purpura is one of the rarest dermatologic manifestations, accounting for 6.4% of all cases with skin manifestations. Retiform purpura, observed exclusively in ill, hospitalized patients, harbors a specific morphology within the spectrum of reticulate eruptions of vascular origin and develops following the compromise of cutaneous blood vessels that result in cutaneous ischemia, purpura, and necrosis4. The pathogenesis of these vascular lesions can be broadly categorized into two main mech- anisms. The first involves vasculitis, material deposition within vessel walls, and vascular wall damage caused by pathogens, whereas the second pertains to vascular occlusion due to thrombosis, embolism, or other clotting abnormalities4. There- fore, skin lesions may develop due to ischemic changes resulting from the occlusion of cutaneous blood vessels caused by a range of factors such as coagulopathy and throm- bosis5. The exact mechanisms underlying the development of coagulopathy and thrombotic events in patients with COVID-19 have not been definitively established. The severe acute respiratory syndrome coronavirus 2 spike protein is proposed to directly activate the complement system, causing endothelial cell injury and thrombosis6. Complement acti- vation can promote coagulation, resulting in overall platelet activation, intravascular platelet aggregation, and fibrin throm- bus formation, ultimately leading to coagulation. Severe COVID-19 is also associated with increased levels of pro- inflammatory cytokines, such as tumor necrosis factor-alpha and various interleukins, which subsequently induce coagu- lation and thrombus formation7. Consequently, in patients with COVID-19, the combination of coagulopathy, thrombus formation, and microangiopathy can lead to various derma- tologic manifestations, including purpura, livedoid purpura, and retiform purpura.
The present case is an example of the increased risk of thromboembolic events associated with COVID-19-induced coagulopathy, leading to the exacerbation of retiform purpura and the development of thromboembolic events, ultimately resulting in cerebral infarction. Given that thromboembolic events are common in patients with severe COVID-197, laboratory parameters such as D-dimer, prothrombin time, platelet count, and fibrinogen should be monitored. In patients with worsening status of these parameters, anticoagulant therapy should be cautiously initiated for both preventive and therapeutic purposes, after excluding other potential bleeding events8. In most patients with COVID-19, systemic or respiratory symptoms tend to emerge before or concur- rently with skin manifestations. However, skin lesions pre- ceding other infection symptoms are relatively rare, accounting for only 12% of all reported cases3. This report highlights a unique and rare presentation of retiform purpura accom- panied by other thromboembolic events, ultimately leading to severe COVID-19 and death.
Retiform purpura might indicate more severe COVID-19. Therefore, in patients with COVID-19 and retiform purpura, early preventive or therapeutic anticoagulation therapy should be considered based on the potential development of throm- boembolic events related to coagulopathy.
References
1. Freeman EE, McMahon DE, Lipoff JB, Rosenbach M, Kovarik C, Desai SR, et al. The spectrum of COVID 19-associated dermatologic manifestations: An international registry of 716 patients from 31 countries. J Am Acad Dermatol 2020;83:1118-1129
Google Scholar
2. Marzano AV, Genovese G, Moltrasio C, Gaspari V, Vezzoli P, Maione V, et al. The clinical spectrum of COVID-19-associated cutaneous manifestations: An Italian multi- center study of 200 adult patients. J Am Acad Dermatol 2021;84:1356-1363
Google Scholar
3. Genovese G, Moltrasio C, Berti E, Marzano AV. Skin mani- festations associated with COVID-19: current knowledge and future perspectives. Dermatology 2021;237:1-12
Google Scholar
4. Georgesen C, Fox LP, Harp J. Retiform purpura: A diag- nostic approach. J Am Acad Dermatol 2020;82:783-796
Google Scholar
5. Bosch-Amate X, Giavedoni P, Podlipnik S, Andreu-Febrer C, Sanz-Beltran J, Garcia-Herrera A, et al. Retiform purpura as a dermatological sign of coronavirus disease 2019 (COVID-19) coagulopathy. J Eur Acad Dermatol Venereol 2020;34:e548-e549
Google Scholar
6. McBride JD, Narang J, Simonds R, Agrawal S, Rodriguez ER, Tan CD, et al. Development of sacral/buttock retiform purpura as an ominous presenting sign of COVID-19 and clinical and histopathologic evolution during severe disease course. J Cutan Pathol 2021;48:1166-1172
Google Scholar
7. Levi M, Thachil J, Iba T, Levy JH. Coagulation abnor- malities and thrombosis in patients with COVID-19. Lancet Haematol 2020;7:e438-e440
8. Thachil J, Tang N, Gando S, Falanga A, Cattaneo M, Levi M, et al. ISTH interim guidance on recognition and management of coagulopathy in COVID-19. J Thromb Haemost 2020;18:1023-1026
Google Scholar
Congratulatory MessageClick here!