pISSN : 3058-423X eISSN: 3058-4302
Open Access, Peer-reviewed

pISSN : 3058-423X eISSN: 3058-4302
Open Access, Peer-reviewed
Yun-ji Lee,Yoonsung Lee,Man S Kim,Bark-Lynn Lew,Soon-Hyo Kwon
10.17966/JMI.2023.28.4.100 Epub 2024 January 04
Abstract
Background: Scabies is a neglected disease that significantly affects the daily lives of patients and their cohabitants.
Objective: To investigate the current epidemiological data regarding scabies in Korea.
Methods: This was a nationwide population-based observational study using data from the National Health Insurance claims database (reference period: 2010~2021). The primary outcome measure was the annual incidence of scabies. Subgroup analyses were performed disaggregated by sex, age, and region of residence.
Results: A total of 517,296 scabies cases were identified, with a male-to-female ratio of 0.83. The annual age-standardized incidence rates steadily decreased from 2010 (97.6 per 100,000 person-years [PY]) to 2021 (43.4 per 100,000 PY), with an average annual percent change of -5.0%. A steep decrease was observed in 2015 (-12.9%), 2020 (-12.7%), and 2021 (-22.8%). An aging trend in patients with scabies was observed, with patients aged ≥50 years accounting for 36.5% and 63.8% of patients in 2010 and 2021, respectively. The ≥80 years age group showed the highest age-specific incidence rate. Although all age groups showed a reduction in annual incidence, the extent of the reduction was relatively greater in patients aged <50 years. The number of patients with scabies was the highest in Gyeonggi, Seoul, and Busan, while the regional incidence rates were highest in Gwangju, Jeonbuk, Jeonnam, Daejeon, and Jeju.
Conclusion: During the last 12 years, there has been a gradual decrease in the overall prevalence of scabies. However, the incidence remains relatively higher among the elderly population.
Keywords
Epidemiology Incidence National Health Insurance Sarcoptes scabiei Scabies
Scabies is a contagious skin disease caused by infestation with the ectoparasite Sarcoptes scabiei var. hominis. The mite burrows and lays eggs under the skin, thus causing severe itch. The condition adversely affects the daily lives of patients and their cohabitants1. Approximately 200 million people suffer from scabies worldwide2. In Korea, scabies accounted for 3.2~9.1% of the outpatient visits at dermatology depart- ments in the 1970s~1980s3. In the 1970s, the spread of scabies most commonly occurred in homes, lodgings, and dormitories. However, since the 1980s, there has been an increased incidence of its spread within long-term care hospitals (LTCHs)4,5. In a multicenter study of Korean patients with scabies (n = 914) conducted in the early 2010s, trans- mission from family members was found to account for 64% of cases, followed by LTCHs (25.7%)6. The most recent epidemiologic study on scabies in Korea was based on the National Health Insurance (NHI) claims database from 2010 to 20177. The study reported the highest annual incidence of 2.9~3.86 per 1,000 people among individuals aged ≥80 years. However, the study did not report age-standardized incidence rates. Moreover, the social distancing measures implemented during the COVID-19 pandemic may have influenced the spread of scabies, since social contact is highly associated with the spread of the disease.
Therefore, the aim of this study was to update the epi- demiological profile of scabies in Korea by analyzing the NHI claims database for the period 2010~2021. Moreover, age-standardized incidence rates (ASRs), to adjust for the effect of an aging population, and regional incidence rates are reported.
This was a nationwide population-based observational study using the NHI claims database which covers up to 98% of the Korean population. Patients with at least one claim record with a diagnostic code (International Classification of Diseases 10th revision) of B86 from 2010 to 2021 were defined as incident cases in the corresponding years. The study population was collected from the resident registration population data released annually by Statistics Korea (http:// kosis.kr).
The primary outcome measure was the annual incidence of scabies between 2010 and 2021. The crude incidence rates (CRs) were calculated as the total number of incident cases divided by the study population in the corresponding years. The study population was divided into 10-year age groups and age-specific incidence rates were calculated by dividing the number of incident cases in the age group by the number of corresponding person-years (PYs). The ASRs were calculated as the sum of the weighted incidence rates for each age group by using Segi's world standard population. The average annual percent change (AAPC) is the weighted average of the annual percent change in the ASRs over a period and was calculated using the formula (exp (b) - 1) × 100, where b is the slope of the regression of the natural log-transformed ASR from the linear regression equation E (log (ASR) | year) = a + b year. Subgroup analysis was per- formed by sex, 10-year age groups (0~9, 10~19, 20~29, 30~39, 40~49, 50~59, 60~69, 70~79, and ≥80 years), and region of residence.
This study was exempted from review by the Institutional Review Board (IRB) of Kyung Hee University Hospital at Gangdong in accordance with the exemption criteria (IRB No. 2023-10-034).
1. Incident cases
Between 2010 and 2021, a total of 517,296 incident cases of scabies were identified. There were 234,255 males and 283,041 females, with a male-to-female ratio of 0.83. The annual number of scabies cases showed a progressive de- crease during the study reference period. The number of scabies cases in 2010 and 2021 were 51,331 and 29,693, respectively, which corresponded to a 42.2% decrease (Fig. 1). A steep reduction (>10%) in the incident cases compared with the preceding year was observed in 2015 (-10.3%), 2020 (-11.2%), and 2021 (-18.8%). The male-to-female ratio steadily decreased from 2010 (0.99) to 2021 (0.64).

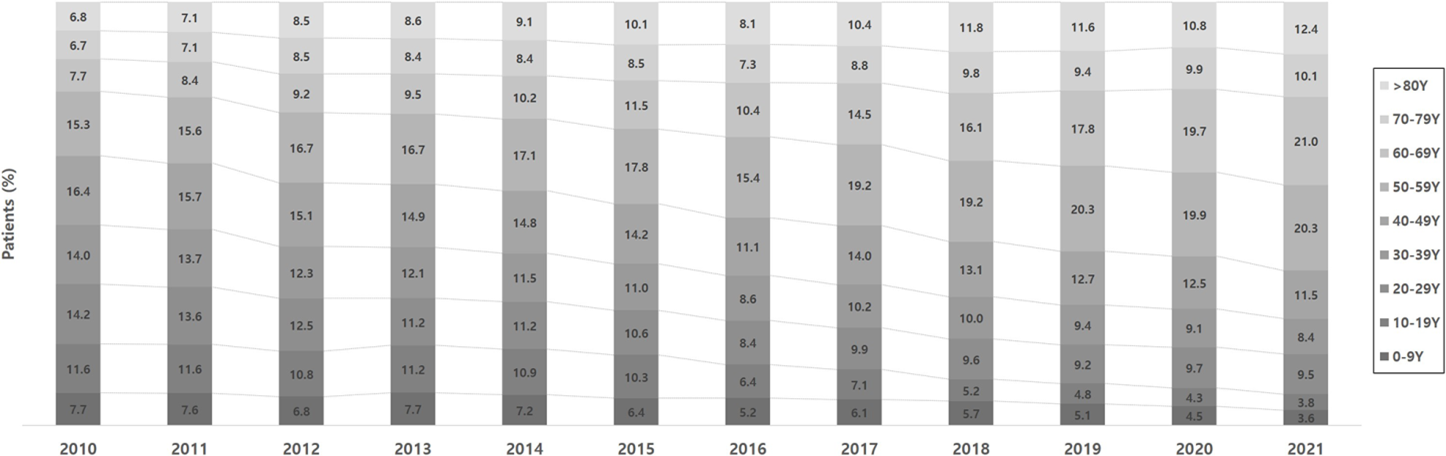
Fig. 2 shows the age distribution of patients with scabies. An aging trend was observed in patients with scabies from 2010 to 2021. In 2010, the 40~49 years age group accounted for the largest proportion of patients (16.4%), followed by the 50~59 years age group (15.3%), 20~29 years age group (14.2%), and 30~39 years age group (14.0%). In 2021, the largest proportion of patients was in the 60~ 69 years age group (21.0%), followed by the 50~59 years age group (20.3%), ≥80 years age group (12.4%), and 40~49 years age group (11.5%). Patients aged ≥50 years accounted for 36.5% of the incident cases of scabies in 2010, and this figure increased to 63.8% in 2021.
2. Crude incidence rate
The annual CR of scabies steadily decreased by 43.8% from 2010 (102.9 per 100,000 PY) to 2021 (57.8 per 100,000 PY) (Fig. 3). A steep decrease in the annual CR (>10%) compared with the preceding year occurred in 2015 (-10.6%), 2020 (-11.2%), and 2021 (-18.8%).

3. Age-standardized incidence rate
The annual ASR of scabies steadily decreased from 2010 (97.6 per 100,000 PY) to 2021 (43.4 per 100,000 PY), with an AAPC of -5.0% (Fig. 4). When the period corresponding to the peak of COVID-19 pandemic (2020~2021) was excluded, the annual ASR showed a decreasing trend from 2010 to 2019 (64.4 per 100,000 PY), with an AAPC of -3.8%. A steep decrease in the annual ASR was observed in 2015 (-12.9%), 2020 (-12.7%), and 2021 (-22.8%).

4. Age-specific incidence rate
The ≥80 years age group showed the highest age-specific incidence rate during the study period, which decreased from 386.1 per 100,000 PY in 2010 to 181.5 per 100,000 PY in 2021 (AAPC, -4.8%) (Fig. 5). In 2010, high incidence rates of scabies were observed in the younger age groups, in- cluding the 20~29 years age group (105.2 per 100,000 PY), 40~49 years age group (96.9 per 100,000 PY), and 10~19 years age group (87.6 per 100,000 PY). By contrast, in 2021, the age groups beyond the threshold of 50 years showed high incidence rates: 60~69 years age group (90.5 per 100,000 PY), 70~79 years age group (81.4 per 100,000 PY), and 50~59 years age group (70.5 per 100,000 PY) had the highest incidence rates following the ≥80 years age group.
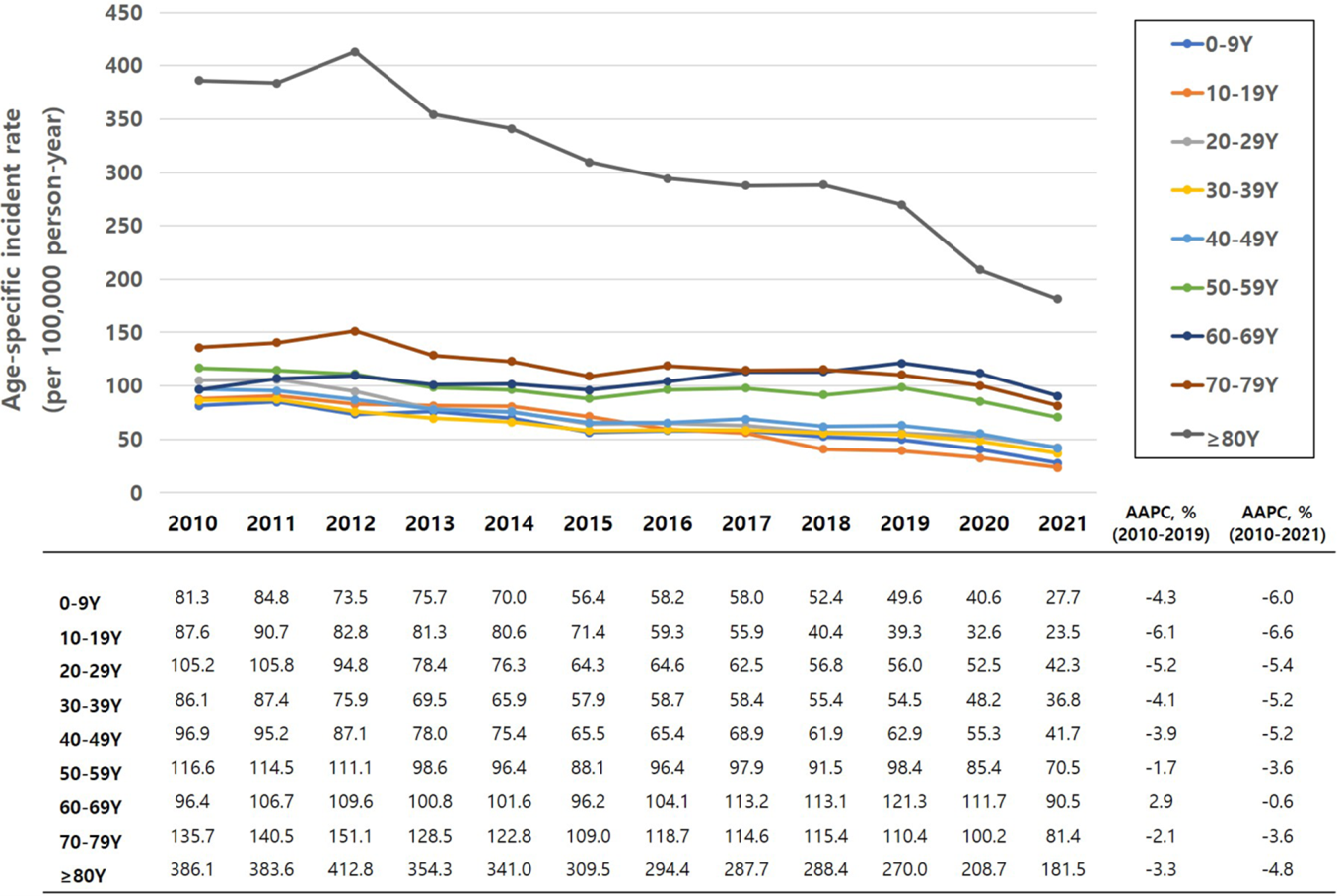
All age groups showed a reduction in incidence rates from 2010 to 2021. However, the extent of reduction was relatively greater in young patients (<50 years) than in old patients (≥50 years): 10~19 years (AAPC, -6.6%), 0~9 years (AAPC, -6.0%), and 20~29 years (AAPC, -5.4%) compared with 60~69 years (AAPC, -0.6%), 50~59 years (AAPC, -3.6%), and 70~79 years (AAPC, -3.6%). Among the age groups be- yond 50 years, the incidence in the 60~69 years age group in 2021 was comparable to that in 2010 (AAPC, -0.6%). After excluding the period corresponding to the COVID-19 pandemic peak, the 60~69 years age group showed an increase in incidence from 96.4 per 100,000 PY in 2010 to 121.3 per PY in 2019, with an AAPC of 2.9%.
5. Regional incidence rate
Fig. 6 shows the regional distribution of patients with scabies. Gyeonggi accounted for the highest proportion of patients during the study period (24.1% in 2010 and 21.3% in 2021), followed by Seoul (17.6% in 2010 and 12.9% in 2021) and Busan (7.3% in 2010 and 8.6% in 2021).

Table 1 shows the regional incidence rates of scabies. In 2010, Gwangju showed the highest incidence (185.2 per 100,000 PY), followed by Jeju (157.6 per 100,000 PY), Jeonnam (139.5 per 100,000 PY), Daejeon (125.7 per 100,000 PY), and Jeonbuk (116.2 per PY). In 2021, these five provinces still had the highest incidence rates: Gwangju (97.0 per 100,000 PY), Jeonbuk (89.0 per 100,000 PY), Jeju (80.9 per 100,000 PY), Jeonnam (80.4 per 100,000 PY), and Daejeon (78.6 per 100,000 PY).
|
|
2010 |
2011 |
2012 |
2013 |
2014 |
2015 |
2016 |
2017 |
2018 |
2019 |
2020 |
2021 |
|
Region, n |
|
|
|
|
|
|
|
|
|
|
|
|
|
Seoul |
88.6 |
91.5 |
81.4 |
75.9 |
68.8 |
60.1 |
65.2 |
66.2 |
58.6 |
62.9 |
54.9 |
40.6 |
|
Busan |
106.7 |
111.2 |
105.8 |
93.2 |
90.9 |
86.2 |
94.3 |
99.3 |
100.0* |
103.9 |
89.4 |
76.6 |
|
Incheon |
102.0 |
98.3 |
96.0 |
87.5 |
84.7 |
73.9 |
72.2 |
76.0 |
76.7 |
70.6 |
60.5 |
53.0 |
|
Daegu |
104.0 |
112.9 |
110.8 |
99.4 |
101.2 |
86.3 |
97.7 |
97.9 |
92.9 |
105.3* |
91.7* |
75.8 |
|
Gwangju |
185.2* |
164.3* |
157.4* |
129.1* |
124.8* |
130.2* |
136.8* |
141.4* |
127.2* |
150.5* |
126.4* |
97.0* |
|
Daejeon |
125.7* |
113.5* |
99.2 |
91.0 |
89.5 |
81.6 |
90.6 |
93.5 |
85.9 |
105.9* |
100.0* |
78.6* |
|
Ulsan |
94.0 |
102.4 |
76.5 |
72.3 |
76.4 |
65.3 |
71.2 |
64.4 |
56.3 |
44.5 |
80.5 |
45.1 |
|
Sejong |
- |
- |
37.7 |
33.4 |
58.6 |
36.7 |
81.9 |
50.3 |
35.5 |
31.6 |
32.0 |
35.8 |
|
Gyeonggi |
106.9 |
110.2 |
99.4 |
85.7 |
83.6 |
69.9 |
70.3 |
69.7 |
70.1 |
68.2 |
63.3 |
47.2 |
|
Gangwon |
91.7 |
112.7 |
131.9* |
114.2* |
102.8 |
119.5* |
112.2* |
102.0* |
91.3 |
86.1 |
79.7 |
75.5 |
|
Chungbuk |
69.1 |
86.6 |
87.3 |
101.9 |
94.8 |
95.0* |
83.3 |
83.2 |
78.6 |
71.3 |
61.1 |
52.1 |
|
Chungnam |
108.5 |
104.5 |
105.8 |
101.1 |
106.5* |
87.6 |
91.1 |
90.4 |
94.6 |
94.8 |
88.3 |
67.0 |
|
Jeonbuk |
116.2* |
134.4* |
116.7* |
102.1* |
101.1 |
91.8 |
100.6* |
115.3* |
117.3* |
130.9* |
96.8* |
89.0* |
|
Jeonnam |
139.5* |
134.7* |
160.3* |
129.7* |
135.4* |
142.0* |
121.8* |
104.5* |
115.1* |
114.2* |
95.2* |
80.4* |
|
Gyeongbuk |
104.5 |
87.7 |
101.6 |
85.5 |
84.3 |
76.9 |
79.7 |
95.1 |
79.8 |
85.8 |
73.9 |
65.2 |
|
Gyeongnam |
90.4 |
99.7 |
79.6 |
93.4 |
108.6* |
91.9 |
91.2 |
98.4 |
81.2 |
87.4 |
74.1 |
67.2 |
|
Jeju |
157.6* |
151.0* |
227.1* |
218.6* |
154.5* |
94.4* |
107.2* |
121.7* |
96.7* |
64.8 |
58.4 |
80.9* |
|
*Top 5
regions where incidence of scabies
was the highest in the corresponding year |
||||||||||||
This nationwide population-based observational study revealed a steady decrease in the incidence of scabies in Korea in all age groups over the last 12 years. Prominent reductions in the incidence of scabies were observed in 2015 and 2020~2021, which corresponded to the outbreaks of the Middle East Respiratory Syndrome (MERS) and COVID-19, respectively. A trend of progressive aging of patients was noted during the study period, with patients aged ≥50 years accounting for 36.5% and 63.8% of cases in 2010 and 2021, respectively. Seoul and Gyeonggi had the highest number of patients with scabies, although the incidence was high in other regions.
The increasing trend of nuclear and single-member families, improved general hygiene, and growing recognition of scabies in LTCHs may have led to a decrease in the incidence of scabies. Given that scabies spreads via close contact, family members and cohabitants of patients are at a high risk of developing scabies. In an analysis of 914 patients with scabies, transmission from a family member was reported in 68% of patients6. In Korea, the phenomenon of nuclear families emerged in the 1990s and became widely prevalent by the early 2010s. Moreover, the number of single-member families in Korea has rapidly increased since the 2010s owing to the trend of delaying or avoiding marriage. The consequent decrease in contact among family members may also have contributed to the decrease in the incidence of scabies.
The two outbreaks of respiratory infectious diseases, namely, MERS in 2015 and COVID-19 in 2020~2021, helped improve the general hygiene practices among the population. During the MERS outbreak, handwashing was emphasized, and social contact was discouraged, thus causing a steep decrease in scabies cases in 2015. However, these results were not sustained after the outbreak, as shown by the comparable incidence of scabies from 2016~2019 to 2015. Owing to the more profound impact of COVID-19 than MERS in terms of its duration and the implementation of social distancing measures, the incidence of scabies was the lowest during the COVID-19 pandemic. Further epidemiological studies on scabies after the COVID-19 pandemic are required to determine whether the dramatic decrease in incidence has been sustained.
The epidemiology of scabies is associated with the socio-economic status of a country. Considering that poor hygiene, overcrowding, and malnutrition are risk factors for scabies, developing countries have a high incidence of scabies in early childhood, and the incidence decreases in adulthood8. By contrast, developed countries have a low incidence of scabies in all age groups2,9. However, localized outbreaks of scabies in LTCHs occur in developed countries with well-established facilities for the elderly. According to a retro- spective analysis, LTCHs accounted for 48% of institutional scabies outbreaks10. The current study revealed a unique epidemiological characteristic of scabies in Korea in that the highest incidence was observed in elderly individuals. The phenomenon of progressive aging of these patients was observed over the last 12 years. In contrast to the even distribution of scabies among individuals aged 20~50 years in the early 2010s, the proportion of elderly patients rapidly increased until 2021. A prominent increase in the proportion of patients was noted in the 60~60 years age group and ≥80 years age group.
The number of LTCHs in Korea has rapidly increased after the initiation of long-term care insurance by the Korean government in 2008. In 2018, the number of registered LTCHs in Korea was 1,450, an increase of 8% each year11. According to a survey, 71.8% of LTCHs in Korea have re- ported scabies cases in the last five years. These outbreaks were attributed to several factors such as delayed diagnosis, lack of separation, shortage of personal protective equipment for personnel, inadequate recognition and health education regarding scabies, and frequent transfer of patients to other facilities or LTCHs. The average duration from the initial pre- sentation of symptoms to the diagnosis of scabies was one week11. Delayed diagnosis might result from nonspecific manifestations or complications, such as secondary bacterial infection in elderly patients, high prevalence of comorbid diseases that impair cognition, and limited diagnostic tools for scabies12. Only 50% of patients with scabies were treated in scabies-restricted rooms, and 32.2% of medical staff who had contact with patients developed scabies because of the insufficient supply of personal protective equipment11.
Although concerns regarding infection control were raised in the early stages, an evaluation conducted in 2011 showed adequate quality control in LTCHs7. The increased recognition of the risk of scabies in LTCHs, particularly among patients and medical staff, has contributed to the decreased incidence of scabies. The Korean government has made concerted efforts to control scabies in LTCHs, including the publication of manuals for the prevention and management of scabies by the Korean Center for Disease Control and the adoption of a reporting system for scabies. Since 2018, hospitals with more than 150 beds are required by law to have infection control rooms with specialized personnel. LTCHs provide regular education about scabies to medical staff, patients, and workers involved in patient care. In 2023, the Korean Dermatologic Association launched the Scabies Control Pro- gram to promote awareness about scabies in the general population, screen for and control scabies in LTCHs, and establish practical guidelines for the diagnosis and manage- ment of scabies1,13.
A subgroup analysis disaggregated by sex showed the predominance of female patients with scabies. The longer average life span, greater sensitivity to itching or skin rashes, and hospital-seeking behavior of females might have con- tributed to this result. In a subgroup analysis disaggregated by region, the highest number of scabies cases was in Seoul and Gyeonggi which have several LTCHs. However, given that these regions have a greater population than other regions, we calculated the regional incidence rates by dividing the number of incident cases by the number of registered residents. A consistently high regional incidence was noted in several provinces during the last 12 years, particularly in Gwangju, Jeonnam, Jeonbuk, Daejeon, and Jeju. Whether scabies is endemic to these regions remains inconclusive, and a detailed study of regional differences in the incidence of scabies is required to validate our results.
Some limitations of our study should be acknowledged. First, the diagnosis of scabies was not universally validated by microscopic investigations or dermoscopy. Both suspected cases of scabies and cases of confirmed or clinically diagnosed scabies were included. Second, prophylactic treatment with gamma-linoleic acid is often provided to all patients in LTCHs once a patient is diagnosed with scabies; this may have led to an underestimation of the number of patients. Third, con- sidering that the registered population number was used as the denominator to calculate regional incidence rates, patients with scabies who visited hospitals outside their registered region of residence could not be counted properly.
This updated report on the nationwide incidence of scabies in Korea revealed a decreasing incidence in all age groups and the aging of affected patients over the last 12 years. Strategies that target elderly patients are required for the effective control of scabies, particularly interventions for con- trolling outbreaks in LTCHs. Outbreaks of respiratory infectious diseases affect the incidence of scabies, thus indicating that general hygiene and isolation are important for scabies control.
References
1. Park J, Kwon SH, Lee YB, Kim HS, Jeon JH, Choi GS. Clinical practice guidelines for the diagnosis and treat- ment of scabies in Korea: Part 1. Epidemiology, clinical manifestations, and diagnosis. Korean J Dermatol 2023; 61:393-403
Google Scholar
2. Karimkhani C, Colombara DV, Drucker AM, Norton SA, Hay R, Engelman D, et al. The global burden of scabies: a cross-sectional analysis from the Global Burden of Disease Study 2015. Lancet Infect Dis 2017;17:1247-1254
Google Scholar
3. Lee WK, Cho BK. [Taxonomical approach to scabies mites of human and animals and their prevalence in Korea]. Korean J Parasitol 1995;33:85-94
Google Scholar
4. Cho BK, Lee JB, Kim CW, Houh W. Clinical study of scabies and itch mite. Korean J Dermatol 1975;13:95-101
5. Yang YS, Lew BL, Sim WY. Clinical study of 27 cases with scabies. Korean J Dermatol 2008;46:1603-1608
6. Park SY, Roh JY, Lee JY, Kim DW, Yoon TJ, Sim WY, et al. A Clinical and epidemiological study of scabies in Korea: A multicenter prospective study. Korean J Dermatol 2014; 52:457-464
7. Kim JH, Cheong HK. Epidemiologic trends and seasonality of scabies in South Korea, 2010-2017. Korean J Parasitol 2019;57:399-404
Google Scholar
8. Romani L, Steer AC, Whitfeld MJ, Kaldor JM. Prevalence of scabies and impetigo worldwide: a systematic review. Lancet Infect Dis 2015;15:960-967
Google Scholar
9. Lassa S, Campbell MJ, Bennett CE. Epidemiology of scabies prevalence in the U.K. from general practice records. Br J Dermatol 2011;164:1329-1334
Google Scholar
10. Mounsey KE, Murray HC, King M, Oprescu F. Retro- spective analysis of institutional scabies outbreaks from 1984 to 2013: lessons learned and moving forward. Epidemiol Infect 2016;144:2462-2471
Google Scholar
11. Kim DH, Yun SY, Park YC, Kang SA, Yu HS. Prevalence of scabies in long-term care hospitals in South Korea. PLoS Negl Trop Dis 2020;14:e0008554
12. Kim HS, Bang JY, Cha KS. A survey on scabies inpatients in South Korea based on health insurance claims data from 2010 to 2019. Healthcare (Basel) 2023;11:841
Google Scholar
13. Park J, Kwon SH, Lee YB, Kim HS, Jeon JH, Choi GS. Clinical practice guidelines for the diagnosis and treat- ment of scabies in Korea: Part 2. Treatment and pre- vention. Korean J Dermatol 2023;21:463-471
Congratulatory MessageClick here!