pISSN : 3058-423X eISSN: 3058-4302
Open Access, Peer-reviewed

pISSN : 3058-423X eISSN: 3058-4302
Open Access, Peer-reviewed
Hui Young Shin,Woo Kyoung Choi,Yu Jeong Park,Ai Young Lee,Seung Ho Lee ,Jong Soo Hong
10.17966/JMI.2023.28.3.68 Epub 2023 October 06
Abstract
Background: Distinguishing verruca plana (VP) from certain types of palmoplantar keratoderma (PPK) can pose challenges as there are few prior investigations.
Objective: This study aimed to enhance the differentiation between VP and PPK by analyzing their clinical characteristics.
Methods: We conducted a retrospective study involving patients diagnosed with VP, or PPK based on biopsy results.
Results: We identified 38 cases with VP/PPK-like lesions on their hands. Among them, ten (26.3%) were diagnosed with VP, while 15 (39.5%) were diagnosed with PPK. VP lesions predominantly manifested on the dorsum of the hand, whereas PPK was primarily observed on the palm, and dorsum. Erythematous, or brownish-colored lesions were more commonly associated with VP, while PPK lesions typically presented as flesh-colored.
Conclusion: By comparing the clinical distinctions between VP, and PPK, we aim to provide valuable insights to facilitate the differentiation of these two conditions, which can sometimes be diagnostically challenging.
Keywords
Differential diagnosis Punctate palmoplantar keratoderma Verruca plana
Verruca plana (VP) is a prevalent dermatological condition caused by infection with the human papillomavirus (HPV). VP predominantly affects children, and young adults. In contrast, palmoplantar keratoderma (PPK) is a rare condition char- acterized by excessive keratin formation on the palms, and soles, resulting in abnormal thickening. Both acquired and inherited forms of these diseases exist.
When the hand exhibits slightly raised papules that raise suspicion of VP, distinguishing it from PPK can be challenging. Morphologically, they can be difficult to differentiate, as VP, and PPK frequently manifest on the hands. However, it is crucial to note that VP is caused by viral infection, and has the potential to spread to other areas of the body or to other individuals if not appropriately treated. Consequently, accurate differentiation between VP, and PPK is essential, particularly when similar lesions occur on the hands. In this study, we aim to compare distinctive clinical features that aid in the differentiation between VP, and PPK.
1. Study design
This retrospective observational study used patient records, biopsy specimens, and clinical images from previously diag- nosed cases of VP, and PPK. The research was conducted on outpatients who visited the Department of Dermatology at Dongguk University Ilsan Hospital between December 1, 2006, and March 30, 2021.
2. Study population, and data collection
Patients who exhibited clinical suspicion of VP, or PPK on their hands, and subsequently underwent a biopsy were enrolled in the study. A total of 38 patients met the inclusion criteria, and demographic information (age, gender), and clinical data (photographs, lesion location, number, and color) were collected. Lesion locations were categorized as dorsum, palm, or both dorsum, and palm. The number of lesions was classified as few (1~5), several (6~10), or multiple (11, and above). Lesion colors were determined through photographic evidence taken during the biopsy, with one case lacking a photograph being excluded from the color analysis. Colors were classified as brown, flesh-colored (including whitish, and yellow), or erythematous.
3. Clinical and histological analysis
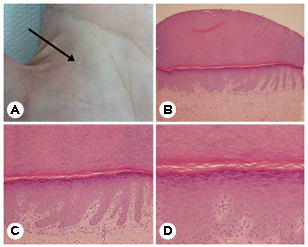
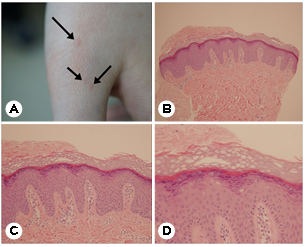
Two experienced dermatologic experts independently analyzed the clinical and histological data. They reviewed, and interpreted the clinical data, histological slides, and photo- graphs of the skin lesions. Skin lesions presenting as flat, slightly elevated papules, or plaques with round, or oval shapes indicated VP. VP lesions may present diffusely, or as individual, or clustered lesions. Those lesions characterized by thickened, and hyperkeratotic papules indicated PPK. PPK may manifest either focally, or diffusely, with prominent scaling, thickening, and hardening of the skin. Histologically, VP is characterized by hyperkeratosis, acanthosis, and distinctive koilocytes with clear perinuclear zones. In contrast, PPK ex- hibits hyperkeratosis, acanthosis, and elongated rete ridges extending into the dermis, with parakeratosis, and the absence of koilocytes distinguishing it from VP.
4. Ethical considerations
This study received approval from the Institutional Review Board of Dongguk University Ilsan Hospital.
5. Statistical analysis
Data collected for this study were analyzed using the SPSS WIN program (Version 21.0), based on the electronic medical records of Dongguk University Ilsan Hospital. An independent-sample t-test was employed for gender after conducting a normality test. The chi-square and Fisher's exact tests were applied to other categorical variables (age, location, number, and color). The significance level for all statistical analyses was set at a p-value less than 0.05.
Of the 38 patients who underwent biopsy, 25 were diag- nosed with either VP, or PPK. Specifically, 15 (39.5%) were diagnosed with PPK, and 10 (26.3%) were diagnosed with VP. Additionally, other skin conditions were observed, in- cluding seborrheic keratosis (5.3%), knuckle pad (5.3%), pitted keratolysis (2.6%), sebaceous hyperplasia (2.6%), for- eign body granuloma (2.6%), pityriasis lichenoides (2.6%), callus (2.6%), chronic granulomatous inflammation (2.6%), and xanthogranuloma (2.6%) (Table 1).
|
Diagnosis |
Number of |
% |
|
Punctate palmoplatar |
15 |
39.5 |
|
Verruca plana |
10 |
26.3 |
|
Granulomatous disease |
3 |
7.9 |
|
Seborrhiec keratosis |
2 |
5.3 |
|
Knuckle pad |
2 |
5.3 |
|
Pitted keratolysis |
1 |
2.6 |
|
Sebaceous hyperplasia |
1 |
2.6 |
|
Pityriasis lichenoides |
1 |
2.6 |
|
Callus |
1 |
2.6 |
|
Nonspecific dermatitis |
2 |
5.3 |
The figures visually represent the clinical features, and pathological findings associated with PPK, and VP. In the photographs, PPK is depicted by flesh-colored papules on the palms. Histologically, PPK is characterized by hyperkeratosis, acanthosis, and elongated rete ridges, with the absence of koilocytes distinguishing it from VP (Fig. 1). In the case of VP, multiple red papules are observed on the dorsum of the hand. Pathologically, mild papillomatosis, hyperkeratosis, and acanthosis are evident, with koilocytes serving as a hallmark feature (Fig. 2).
Regarding the distribution of patients by sex, 15 were female, and 10 were male (Table 2). The age range of the patients spanned from 2 to 64 years, with a mean age of 38.8 years. Most participants fell into the age groups of their 30s (23.7%), and 50s (23.7%), followed by those in their 40s (21.1%), and 20s (15.8%) (Table 3). Demographic characteristics, including sex, and age, did not exhibit significant differences between the VP, and PPK groups.
|
VP (n=10), |
PPK (n=15), |
p* |
|
|
Gender‡ |
|||
|
Male |
6 (60.0) |
4 (26.7) |
0.122 |
|
Female |
4 (40.0) |
11 (73.3) |
|
|
Age, years† |
|
|
|
|
(mean ± SD) |
35.8±18.2 |
44.1±8.6 |
0.206 |
|
Location‡ |
|||
|
Dorsum |
9 (90.0) |
2 (13.3) |
0.000* |
|
Palm |
0 (0.0) |
9 (60.0) |
|
|
Whole |
1 (10.0) |
4 (26.7) |
|
|
Number of lesions‡ |
|||
|
Few (1~5) |
3 (30.0) |
3 (20.0) |
0.724 |
|
Several (6~10) |
0 (0.0) |
2 (13.3) |
|
|
Multiple |
7 (70.0) |
9 (60.0) |
|
|
No photo |
0 (0.0) |
1 (6.7) |
|
|
Color‡ |
|||
|
Flesh (Skin-colored,
whitish or yellowish) |
0 (0.0) |
12 (80.0) |
0.000* |
|
Brownish |
3 (30.0) |
1 (6.7) |
|
|
Erythematous |
7 (70.0) |
1 (6.7) |
|
|
No photo |
0 (0.0) |
1 (6.7) |
|
|
*Significantly different between the VP and PPK groups (p-value<0.05) †Continuous
variable: Independent sample t-test was per formed because the normality test result showed
normality. ‡Categorical
variables: chi-square test (Fisher's exact test) |
|||
|
Age |
Number of patients (%) |
|
1~20 |
4
(10.6) |
|
21~30 |
6
(15.8) |
|
31~40 |
9
(23.7) |
|
41~50 |
8
(21.1) |
|
51~60 |
9
(23.7) |
|
≥61 |
2
(5.3) |
In VP cases, the majority (90.0%) presented lesions on the dorsal aspect, with a smaller percentage (10.0%) displaying lesions on both the palm, and dorsum of the hand. Conversely, the most common location for PPK was the palm (60.6%), followed by involvement of the entire hand, including the palm, and dorsum (26.7%), and dorsal involvement (13.3%). Regarding lesion location, VP tended to occur more frequently on the dorsum than PPK, while PPK was significantly more prevalent on the palms than VP. The number of lesions was predominantly multiple in both the PPK (60.0%), and VP (70.0%) groups, with no significant difference between them (Table 2).
Regarding lesion color, erythematous was the most com- mon color in VP cases (70.0%), followed by brown (30.0%), with no occurrences of flesh-colored lesions. In PPK, lesions were primarily flesh-colored (80.0%), followed by brownish, and erythematous lesions (6.7%). The erythematous color was significantly more common in the VP group, whereas PPK was notably more associated with flesh-colored lesions (Table 2).
VP is a well-known dermatological condition caused by HPV infection. It commonly manifests on the hands, feet, and face, often causing cosmetic concerns1,2. VP is frequently seen in children and young adults and is characterized by multiple flat areas with a slightly raised surface compared to normal skin, typically small in size (less than 5 mm)3. Untreated VP can spontaneously clear, but it may persist and spread to adjacent skin or other individuals4.
On the other hand, PPK represents a group of acquired and hereditary disorders characterized by excessive thickening of the epidermis, usually manifesting from birth or childhood5. PPK is categorized into four morphological patterns: (i) diffuse, (ii) focal, (iii) striate, and (iv) punctate6,7. Certain forms of PPK, especially the striate or punctate variants, present with multiple thickened hyperkeratotic plaques or papules on the hands and feet, which can resemble VP.
Despite morphological similarities, it is imperative to dis- tinguish between VP and PPK due to their differences in etiology, contagiousness in the case of VP, and variations in treatment approaches1.
According to our study involving 38 patients who under- went biopsy, 25 received diagnoses of either VP or PPK; 10 patients (26.3%) were diagnosed with VP, and 15 (39.5%) with PPK. Although VP is generally more prevalent than PPK, our study observed a higher incidence of PPK diagnoses. It is important to note that our study focused exclusively on patients with hand lesions, and biopsies were performed when diagnoses were uncertain, which may have contributed to the higher number of PPK cases.
Our findings regarding the ages of patients with VP and PPK deviate from typical age distributions. Mastkar et al. reported an average age of 21.6 years8 for VP patients, whereas PPK is typically associated with a younger age at onset. In our study, the average age for VP patients was 43.2 years, and for PPK patients, it was 35.8 years, with the majority falling within their 30s and 40s. This discrepancy could be attributed to our study’s unknown exact time of onset, with diagnoses primarily relying on histological examination.
With regard to lesion location, VP was predominantly ob- served on the dorsum (90%), while PPK was primarily noted on the palms or the entire hand (86.7%). The characteristic location of VP on the dorsum is linked to its potential for spreading through direct contact due to HPV infection. In contrast, often hereditary, PPK tends to manifest at pressure-bearing sites. It can affect the entire palmoplantar surface as diffuse PPK or localize to the palm under pressure, extending throughout the hand as focal or punctate PPK.
Differences in lesion color were also evident, with VP lesions primarily being brown (30%) or erythematous (70%), where- as PPK lesions were predominantly flesh-colored (80%). No significant differences were observed in terms of lesion numbers.
A comparative analysis of clinical characteristics, including age distribution, location, and color, can be instrumental in diagnosis. The primary aim of our study was to analyze the clinical characteristics of VP and PPK, recognizing the inherent difficulty in distinguishing between them.
Our study has limitations, including the relatively small sample size due to its focus on patients with suspected VP or PPK on the hands confirmed by biopsy. Additionally, due to data limitations, a comprehensive exploration of illness duration and family medical history was impossible. Notably, our study did not differentiate between acquired and her- editary forms of PPK. The retrospective data collection may introduce bias. Nonetheless, to our knowledge, this is the first study to compare the clinical characteristics of VP and PPK affecting the hand. Furthermore, the emerging field of dermoscopy holds promise in aiding the differentiation of these two diseases, warranting further investigation.
In conclusion, our clinical review of 38 patients who under- went biopsy for hand lesions resembling VP and PPK reveals distinctions in clinical characteristics between these two con- ditions. VP is commonly found on the dorsum and typically presents as brownish or erythematous lesions, while PPK primarily affects the palms or entire hands and exhibits a predominantly flesh-colored appearance. The hand is a con- spicuous site for identifying various skin lesions, with VP and PPK representing characteristic diseases that can manifest in this region9,10. These findings are anticipated to be valuable in scenarios where papular lesions pose diagnostic challenges. These clinical distinctions can facilitate differentiation and guide appropriate treatment decisions in cases where biopsy is unfeasible.
References
1. Witchey DJ, Witchey NB, Roth-Kauffman MM, Kauffman MK. Plantar warts: epidemiology, pathophysiology, and clinical management. J Am Osteopath Assoc 2018;118: 92-105
Google Scholar
2. Kiyofumo E. HPV-associated cutaneous lesions. Uirusu 2008;58:173-182
Google Scholar
3. Sterling JC. Human papilloma virus infection. In: Kang S, Amagai M, Bruckner AL, Enk AH, Margolis DJ, McMichael AJ, et al. editors. Fitzpatrick's dermatology in general medicine. 9th ed. New York: McGraw Hill, 2022:3095-3100
4. Kyriakis KP, Pagana G, Michailides C, Emmanuelides S, Palamaras I, Terzoudi S. Lifetime prevalence fluctuations of common and plane viral warts. J Eur Acad Dermatol Venereol 2007;21:260-262
Google Scholar
5. Has C, Technau-Hafsi K. Palmoplantar keratodermas: clinical and genetic aspects. J Dtsch Dermatol Ges 2016; 14:123-139
Google Scholar
6. Guerra L, Castori M, Didona B, Castiglia D, Zambruno G. Hereditary palmoplantar keratodermas. Part I. Non-syndromic palmoplantar keratodermas: classification, clinical and genetic features. J Eur Acad Dermatol Venereol 2018;32:704-719
Google Scholar
7. Guerra L, Castori M, Didona B, Castiglia D, Zambruno G. Hereditary palmoplantar keratodermas. Part II: syndromic palmoplantar keratodermas - Diagnostic algorithm and principles of therapy. J Eur Acad Dermatol Venereol 2018; 32:899-925
Google Scholar
8. Masatkar V, Gupta LK, Khare AK, Mehta S, Mittal A. Clinicoepidemiologic study of verruca plana at a tertiary care center. Indian J Dermatol Venereol Leprol 2018;84: 247
Google Scholar
9. Hongal AA, Rajashekhar N, Gejje S. Palmoplantar Dermatoses- A Clinical Study of 300 Cases. J Clin Diagn Res 2016;10:WC04-WC07
Google Scholar
10. Kang BS, Lee JD, Cho SH. A clinicopathological study of palmoplantar dermatoses. Korean J Dermatol 2006;44: 714-720
Google Scholar
Congratulatory MessageClick here!