pISSN : 3058-423X eISSN: 3058-4302
Open Access, Peer-reviewed

pISSN : 3058-423X eISSN: 3058-4302
Open Access, Peer-reviewed
Sang-Doo Lee,Min Kyung Shin
10.17966/JMI.2023.28.1.1 Epub 2023 April 05
Abstract
Background: Oral antifungal drugs are the primary treatment for onychomycosis. However, there are few studies on the effectiveness and safety of oral combination therapy after laser treatment.
Objective: We sought to contrast the efficacy and safety of laser and oral combination therapy with that of oral monotherapy for non-responders to laser treatment.
Methods: We retrospectively evaluated the medical charts and photographs of 20 patients who received four sessions of Nd:YAG laser. Among these patients, 11 were "laser non-responders" and 9 were "laser partial responders". Afterward, 10 patients received oral drugs in addition to laser treatment (combination therapy) and the other 10 were completely altered to oral drugs, with no laser treatment (oral monotherapy). Clinical evaluation was conducted at baseline and 3 months after treatment. Recurrence was evaluated 3 months after the final evaluation.
Results: Clinical evaluation revealed that combining or switching to oral antifungal drugs was substantially effective in the laser non-responder group (Z = -2.481, p = 0.013). Combination therapy was more effective than oral monotherapy (Z = -1.324, p = 0.247). Furthermore, positive baseline mycological results demonstrated a higher possibility of laser monotherapy failure (χ2 = -5.089, p = 0.024). There were two cases of recurrence in the oral monotherapy group and no adverse effect was discovered in any patient.
Conclusion: This study highlighted that the combination of oral drugs with laser therapy could be beneficial regarding efficacy, recurrence, and safety in the treatment of patients who are refractory to laser therapy.
Keywords
Fungal infection Nd:YAG laser Onychomycosis Oral antifungal drug PinPointe laser
Onychomycosis is a typical nail disease, accounting for 50% of abnormal nails1. It is prominent in South Korea, causing 10% of all dermatological out-patient cases2. The major treatment options include topical and oral antifungal medications. Single topical agents are inadequate for onycho- mycosis because they exhibit limited penetration to the nail plate. Oral antifungal therapies are found to be the most effective treatment options; however, they have limited use due to slow responses, high recurrences, and adverse effects, with a failure rate of about 30%3. Meanwhile, the appli- cation of laser treatment continues to gain attraction as an alternative treatment option with many advantages, such as relatively fast response, fewer side effects, and avoidance or mitigating the duration of oral therapy4. Among the several laser equipment types, the 1,064-nm neodymium-doped yttrium aluminum garnet (Nd:YAG) laser is a laser device that reaches the nail plate and bed, facilitating superheating of the fungal materials and suppressing their growth5. However, some patients are refractory to laser monotherapy. Thus, combination therapy has garnered considerable interest, given its potential for drug synergy and prevention of antifungal resistance6. To date, few analyses have contrasted the com- bination of laser and oral drugs with oral monotherapy for laser non-responders after different cycles of laser treatment, offering clinicians guidance on whether it is better to combine oral drugs with laser treatment or entirely switch to oral drugs if laser treatment fails. Therefore, we undertook this retrospective study to assess the efficacy and safety of oral drug intervention for non-responders to laser therapy and compare the efficacy of the integration of laser and oral drugs with that of oral monotherapy.
1. Study population
A retrospective review of electronic charts was conducted for patients with onychomycosis, who visited the Department of Dermatology at Kyung Hee University Medical Center between September 2021 and September 2022, and were treated with Nd:YAG laser for at least four sessions (PinPointe foot laser, CYNOSURE, US) and were subsequently switched to oral drugs or continued laser treatment combined with oral drugs. We analyzed the records of 72 patients. The research was authorized by the Institutional Review Board of the hospital (2021-09-034) and was executed following the principles of the Declaration of Helsinki.
Patients were exempted based on the following criteria: irregular visits, much far from the visit interval, termination of treatment by the patient, inadequate data for photographs, oral antifungal therapy within 6 months before the study, nail discoloration facilitated by factors other than a fungus or Candida, and psoriasis and lichen planus of the nail plate. After applying the exclusion criteria, 52 patients were screened, and finally, 20 patients were enrolled in the study.
2. Study design
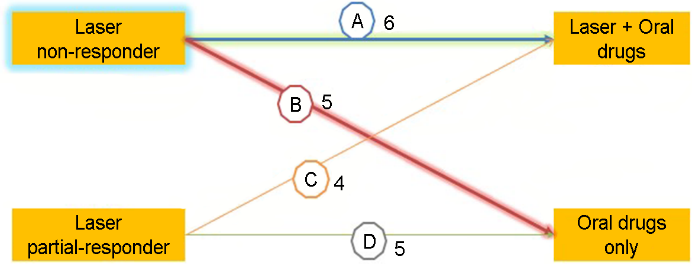
The final 20 patients were categorized into two groups based on the investigator's global assessment (IGA) re- sponse7: the laser non-responder group and the laser partial-responder group. The laser non-responder group comprised older patients with an IGA score of 0 (worse, deterioration from baseline) or 1 (poor, <24% improvement) after four sessions of laser treatment, whereas the laser partial-responder group comprised nine patients with IGA scores of 2 (fair, 25~49% improvement), 3 (good, 50~89% improvement), and 4 (excellent, 90~99% improvement). No patient had an IGA score of 5 (cleared, 100% remission except for residual manifestations) that conformed to the absence of demand for additional oral treatment. Ten patients received oral anti- fungal drugs in combination with the ongoing laser therapy, and the other ten patients were switched to oral drugs with no additional laser sessions, as illustrated in Fig. 1.
Concerning the laser treatment protocol, nails thicker than 2 mm were mechanically debrided using a nail grinder before treatment. The parameter settings of the laser were wave- length, 1,064 nm; pulse energy, 200 mJ; pulse duration, 0.1 ms; spot size, 1.5 mm; frequency, 30 Hz, and temperature, 40~60℃. The laser beam was moved spirally to cover the entire nail plate. The procedure was conducted twice following a 2-min pause. The patients were treated at 1-month intervals for a total of four sessions.
For oral therapy, three antifungal drugs were given, with a dose was 250 mg a day of terbinafine, 200 mg a day of itraconazole, and 150 mg a week of fluconazole. In the aspect of itraconazole, two patients were treated with pulse therapy comprising 200 mg twice daily for 1 week followed by a 3-week off. Terbinafine was given to most patients (15/20), followed by itraconazole (3/20) and fluconazole (2/20).
3. Outcome assessment
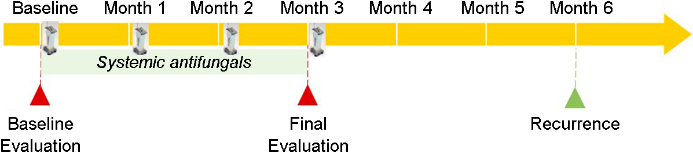
The major outcome of this study was to evaluate clinical efficacy by calculating IGA response based on modifications in the onychomycosis severity index (OSI)7,8. The OSI scoring system highlights the infected area, proximity to the nail matrix, dermatophytoma, and subungual hyperkeratosis8. To demonstrate statistically significant improvement, a clinical cure was outlined as IGA scores 3, 4, and 5, which indicates an improvement of more than 50%. For baseline mycological evaluation, four different modalities were conducted: fungus culture, potassium hydroxide (KOH) smear, nail periodic acid schiff (PAS), and reflectance confocal microscopy (RCM). We deemed the outcome of mycological evaluation as "positive" if at least one test revealed a positive result, considering the high specificity and relatively low sensitivity of each test9. Outcome evaluations were conducted at baseline and 3 months after treatment. 3 months after the final analysis, the patients were asked to visit the hospital to detect recurrence, which was defined as the emergence of clinical evidence of infection, considering color change, thickness, and dermato- phytoma. The entire process and the evaluation period are depicted in Fig. 2. Furthermore, we attempted to determine the factors influencing laser treatment failure. Important variables included age, sex, chronic illness, concomitant drugs, nail site, clinical type, and baseline mycological evaluation.
4. Safety evaluations
Patients were asked to mention any adverse effects at all follow-up visits, ranging from baseline evaluation to 6 months.
5. Statistical analysis
All statistical analyses were conducted using SPSS software (version 20.0; SPSS Inc., Chicago, IL, USA). Because the pro- portion of patients is less than 30, we applied Wilcoxon Signed-Rank Test to contrast clinical improvement between the intervention modalities of oral therapies and the Mann-Whitney U-test to assess combining therapy and oral monotherapy in the laser non-responder group. Furthermore, we employed a chi-square test to determine factors affecting the output of laser treatment. Statistical significance was set at p-value < 0.05.
1. Demographic information
Twenty patients were chosen according to the inclusion criteria. The mean age of the patients was 55.2 (± 12.4) years. The most widespread chronic illness was urticaria equally accompanied by hypertension and diabetics mellitus (DM) and the most predominantly co-used drug was an antihistamine. The total number of affected nails was 99, with an average of 4.9 nails per patient, and the great toenail was the most constantly affected. The most prevalent clinical type was distal lateral subungual onychomycosis (14/20 patients). All patients were treated with topical efinaconazole. According to the presumption of the baseline mycological evaluation presented above, 14 patients demonstrated mycologically positive results, which were, when we assess them more exclusively, 11 positivity of KOH, 6 positivity of fungus culture, and 7 positivity of PAS or RCM. The most predominant species discovered by fungus culture was Tinea rubrum (3/7), followed by Fila- mentous fungi (2/7). The demographic information of the patients categorized according to treatment modalities is presented in Table 1.
|
|
Laser
non-responders |
|
Laser
partial responders |
χ2 |
p value |
||
|
Laser + |
Oral |
Laser + |
Oral |
||||
|
Patients |
6 |
5 |
|
4 |
5 |
|
|
|
Men |
0 |
2 |
|
1 |
0 |
0.194 |
0.660 |
|
Women |
6 |
3 |
|
3 |
5 |
|
|
|
Age (years, mean ± SD) |
55.5±9.0 |
49±21.3 |
|
56.5±7.0 |
60±7.8 |
1.401 |
0.705 |
|
Chronic illness |
3 |
0 |
|
4 |
3 |
3.039 |
0.081 |
|
DM |
|
|
|
1 |
|
|
|
|
Hypertension |
1 |
|
|
1 |
|
|
|
|
Dyslipidemia |
1 |
|
|
1 |
|
|
|
|
Urticaria |
1 |
|
|
|
2 |
|
|
|
Eczema |
|
|
|
|
1 |
|
|
|
HBV carrier |
|
|
|
1 |
|
|
|
|
Concomitant drugs |
3 |
2 |
|
3 |
4 |
1.650 |
0.199 |
|
Isotretinoin |
|
1 |
|
|
|
|
|
|
Doxycycline |
|
1 |
|
|
|
|
|
|
Antihistamines |
1 |
|
|
|
3 |
|
|
|
Immunosuppressants |
|
|
|
|
1 |
|
|
|
Statin |
1 |
|
|
1 |
|
|
|
|
HTN medication |
1 |
|
|
1 |
|
|
|
|
DM
medication |
|
|
|
1 |
|
|
|
|
Unknown |
|
|
|
|
|
|
|
|
Nail location |
|
|
|
|
|
2.888 |
0.236 |
|
Great
toenail |
5 |
8 |
|
8 |
7 |
|
|
|
Other
toenail |
3 |
24 |
|
24 |
12 |
|
|
|
Fingernail |
6 |
0 |
|
0 |
0 |
|
|
|
Clinical type |
|
|
|
|
|
1.299 |
0.522 |
|
DLSO |
5 |
3 |
|
2 |
4 |
|
|
|
TDO |
1 |
2 |
|
1 |
1 |
|
|
|
PSO |
0 |
0 |
|
1 |
0 |
|
|
|
Baseline mycologic |
5/6 |
5/5 |
|
2/4 |
2/5 |
5.089 |
0.024† |
|
Oral antifungal drugs |
|
|
|
|
|
|
|
|
Terbinafine |
4 |
4 |
|
2 |
5 |
|
|
|
Itraconazole |
1 |
1 |
|
1 |
0 |
|
|
|
Fluconazole |
1 |
0 |
|
1 |
0 |
|
|
|
No
significant differences were detected between the groups concerning sex, age,
chronic illness, concomitant drugs, site of †Statistically
significant at p < 0.05 |
|||||||
2. Comparison of the impact of oral antifungal intervention between laser non-responders and partial responders
Eleven laser non-responders and nine laser partial re- sponders were measured to determine the influence of oral therapies. In the laser non-responder group, merging with or switching to oral antifungal drugs was considerably effective in a clinical evaluation with the elevation of mean IGA from 0.82 to 2.09 (Z = -2.481, p = 0.013). The clinical cure rate, which is the percentage of patients achieving a predefined clinical cure, rose from 0% to 45.5% after oral therapies. In contrast, the laser partial-responder group did not attain a statistically significant change (Z = -0.707, p = 0.480). The change in mean IGA indicated a decline of 0.3, which implies an ironically partial deterioration after an oral intervention.
3. Comparison between combining and switching to oral treatments in the laser non-responder group
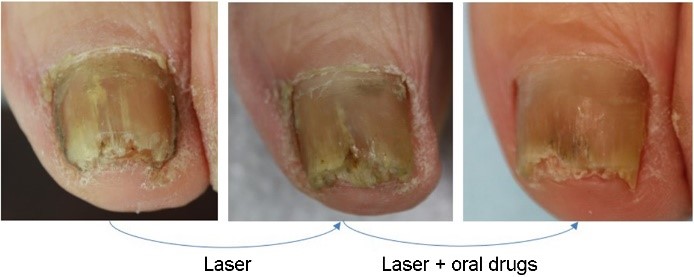
Among the 11 laser non-responders, 6 patients were treated with combination therapy (laser plus oral antifungal drugs), while the other 5 were treated with oral monotherapy. Patients who received combination therapy demonstrated a 2.5 increase in the mean IGA score, but those who received oral monotherapy expressed only an increase of 1.6 (Fig. 3). This implied that combining oral drugs was more efficient than explicitly switching to oral drugs from laser treatment alone, although this was not statistically significant (Z = -1.324, p = 0.247). The comprehensive IGA responses based on the OSI are highlighted in Table 2.
|
Group |
Patient |
OSI |
|
IGA
response† |
|||||
|
Before
oral intervention (Laser
only) |
|
After
oral |
Before
oral intervention |
After oral |
|||||
|
Before |
After |
Before |
After |
B/A*100 |
D/C*100 |
||||
|
Laser + Oral drug |
1 |
12 |
12 |
|
25 |
16 |
|
0 |
2 |
|
2 |
35 |
35 |
|
35 |
35 |
|
0 |
0 |
|
|
3 |
22 |
22 |
|
12 |
6 |
|
1 |
3 |
|
|
4 |
30 |
25 |
|
25 |
12 |
|
1 |
3 |
|
|
5 |
8 |
8 |
|
8 |
1 |
|
1 |
4 |
|
|
6 |
26 |
22 |
|
30 |
14 |
|
1 |
3 |
|
|
Oral |
7 |
9 |
6 |
|
6 |
4 |
|
1 |
2 |
|
8 |
30 |
30 |
|
30 |
30 |
|
1 |
1 |
|
|
9 |
6 |
4 |
|
4 |
6 |
|
1 |
0 |
|
|
10 |
26 |
22 |
|
4 |
1 |
|
1 |
3 |
|
|
11 |
30 |
26 |
|
35 |
19 |
|
1 |
2 |
|
|
OSI, Onychomycosis severity index;
IGA, Investigator's global assessment †IGA response was
determined by the value corresponding to when the calculated outputs were
within the following |
|||||||||
4. Factors affecting failure of laser treatment
We could not detect any statistically significant factor influencing the output of laser treatment regarding sex, age, chronic illness, concomitant drugs, number, site of affected nails per patient, and clinical type. However, we determined statistical significance in baseline mycological analysis, of which the positive result denoted a higher likelihood of failure of laser treatment (χ2 = 5.089, p = 0.024).
5. Adverse events
Regarding safety, no particular adverse events occurred. There were two cases of recurrence only in patients treated with switching therapy and none in those treated with combined therapy.
The treatment of onychomycosis primarily includes oral and topical antifungal drugs10. A single topical antifungal drug is inadequate for the complete removal of the fungus, and oral antifungal drugs are strongly demanded not only for their supportive and synergistic effect with the topical agent but also for application as a single therapy11. However, their long-term use is minimized when patients are immunocom- promised, hepatopathic, nephropathic, or poly medicated. Furthermore, not every patient is satisfied with their efficacy. Oral antifungal drugs are known to be potent in eradicating fungi, meaning they have a good fungicidal effect; however, they are ineffective in attaining rapid and long-lasting clinical improvement, including nail color and thickness12,13. Despite the excellent mycological cure rate linked to oral antifungal drug use, a 5-year follow-up study revealed that 53% and 23% of the patients who achieved mycological cure at 12 months after oral itraconazole and terbinafine, respectively, had mycological relapse or reinfection14.
Lately, several studies have attempted to substitute this treatment with laser treatment to improve the cure rate, reduce adverse effects, and eliminate drug-resistant patho- gens. Although there are different types of lasers available, 1,064 nm Nd:YAG laser therapy is simple, quick, minimally invasive, and comparably well tolerated5,15. The laser is also conducive for multiple fungal species16. Unlike Q-switched or short-pulse Nd:YAG lasers, long-pulse (ms) Nd:YAG laser has been studied extensively and is known to indicate a mycological cure rate of more than 70% and a clinical cure rate of 50% after 6 months of treatment17. Based on these similar robust research outputs, the Ministry of Food and Drug Safety in South Korea authorized the use of a long-pulse 1,064 nm Nd:YAG laser for onychomycosis17. A retrospective study of 30 patients with onychomycosis proposed that the Nd:YAG laser offers effective treatment, as demonstrated by its significant mycological and clinical clearance18. However, some patients remain refractory to laser monotherapy. A review of 24 laser trials on onychomycosis revealed that there was little evidence supporting the use of lasers for clinical cure19. In a systematic review of 25 randomized controlled trials on laser monotherapy, a complete cure was not found in any study, and mycologic cure was examined in only one study20. Furthermore, laser treatments are not cheap, are generally not insured, and typically require multiple monthly or biweekly sessions21. Therefore, it is essential to integrate laser treatments with other interventions.
Studies comparing laser and oral combination therapies with oral monotherapy are meager. A recent study by Khater et al. evaluated the efficacy of combined Nd:YAG laser treat- ment and itraconazole versus that of itraconazole solely and indicated that clinical cure expressed better results in group II (laser and itraconazole) than in group 1 (itraconazole alone). However, the mycological cure did not reveal a substantial difference between the groups22. In 2016, Li et al. described that a combination of itraconazole and laser therapy was suggested for severe onychomycosis, whereas single medi- cation and combination treatments revealed no difference in patients with mild or moderate onychomycosis23. In 2014, Xu et al. indicated that combined treatment was better than either oral therapy or laser treatment and was particularly effective in the first 3 months of treatment12.
First, we equipped the study to present evidence that add- itional oral drugs benefit laser non-responders more than partial laser responders. Consistent with our expectations, regardless of the method of oral intervention, both combination and oral monotherapy were substantially effective only for non-responders. This implies that patients who are satisfied with laser treatment even slightly are better able to keep it up, instead of considering other options. However, in cases where a patient does not appear to be the right fit for laser therapy, integrating and switching to oral drugs may be a good alternative option.
Second, we attempted to identify whether combining or switching to oral drugs was preferable for laser non-responders, and our analysis showed that combining oral drugs seemed to be superior to switching to oral drugs alone. Two cases of recurrence occurred only in the oral monotherapy group. The mechanism of long-pulsed Nd:YAG lasers are not exten- sively known; however, different hypotheses have been pro- posed. Local hyperthermia influences protein denaturation and fungal apoptosis. Furthermore, laser waves are selectively absorbed by melanin on fungal cell walls, thus inhibiting fungal growth and influencing the growth of infected nails23. An in vitro study revealed that a long-pulsed 1,064-nm Nd:YAG laser can effectively hinder the growth of Tinea rubrum24. In contrast, oral antifungal drugs inhibit the activity of sterol 14α demethylase, which can obstruct the synthesis of ergosterol, a crucial component of fungal cell membranes23. Considering the different mechanisms of action, the syner- gistic impacts of oral drugs and lasers appear to play no role in improving efficacy and reducing recurrence. Therefore, it is rational to presume that combination therapy can shorten the treatment duration of oral drugs and achieve broader antifungal coverage while preserving the same efficacy25. A large-scale systematic review in 2022 demonstrated a signifi- cant clinical benefit of laser and oral combination therapy over monotherapy in almost all studies (14/15, 93.3%)6.
Despite the many advantages of combination therapy over monotherapy, there are still some safety issues. The above-mentioned systematic review revealed that there was a greater number of studies on the adverse events linked to combination therapy than with monotherapy6. Most adverse events were mild-to-moderate burning sensation and pain. However, most sample sizes were small, and the monotherapy comprised a topical drug or placebo, not an oral drug. It is obscure whether the adverse events were linked to the combinational effect of treatment or the procedure itself, like the super- heating by the high thermal energy of the laser. No severe adverse events, except for the temporary elevation of hepatic function, were observed in any of the studies on the com- bination therapy of laser and oral drugs12,22,23. In our study, no explicit adverse events occurred in either group. Therefore, combination therapy is generally well accepted.
Furthermore, we attempted to determine several differential points for distinguishing laser responders from laser non-responders. The baseline mycological result was the only substantial factor that impacted the effectiveness of laser treatment. Therefore, when we discover a patient whose baseline mycological evaluation is negative, but who is clinic- ally and circumstantially believed to be an onychomycosis patient, we would be more encouraged to consider laser treatment.
This study had several limitations, including the small proportion of cases, incomplete mycological data, uneven distribution of sex, clinical types, and application of antifungal oral drugs with different cure rates, which can be attributed to the inherent characteristic of this retrospective study. We had to use a non-parametric statistic test because of the small number of patients less than 30. We mostly relied on clinical clues highly indicative of onychomycosis to validate the diagnosis of onychomycosis without conducting myco- logical examinations for all patients; however, the risk of misdiagnosis was lowered by excluding possible differential diagnoses, such as nail lichen planus and psoriasis, during patient screening10. Furthermore, this study tracked recurrence for only 6 months. Considering the high recurrence rate of oral monotherapy, studies with longer follow-ups are required to optimize treatment regimens14. Based on this analysis, a prospective study designed to complement such limitations will be required soon.
Laser treatment is particularly beneficial for older, immuno- compromised, uncontrolled DM, hepatopathic and nephro- pathic patients, for whom long-term oral drugs could pose some risk. However, when a patient is refractory to laser therapy, integrating oral drugs with laser therapy could be beneficial for efficacy, recurrence, and safety.
References
1. Finch JJ, Warshaw EM. Toenail onychomycosis: current and future treatment options. Dermatol Ther 2007;20: 31-46
Google Scholar
2. Hwang SM, Kim DM, Suh MK, Kwon KS, Kim KH, Ro BI, et al. Epidemiologic survey of onychomycosis in Koreans: Multicenter study. Korean J Med Mycol 2011;16:35-43
Google Scholar
3. EI-Tatawy RA, Abd EI-Naby NM, EI-Hawary EE, Talaat RAZ. A comparative clinical and mycological study of Nd-YAG laser versus topical terbinafine in the treatment of onycho- mycosis. J Dermatolog Treat 2015;26:461-464
Google Scholar
4. Zhang RN, Wang DK, Zhuo FL, Duan XH, Zhang XY, Zhao JY. Long-pulse Nd:YAG 1,064-nm laser treatment for onychomycosis. Chin Med J 2012;125:3288-3291
Google Scholar
5. Gupta A, Simpson F. Device-based therapies for onycho- mycosis treatment. Skin Therapy Lett 2012;17:4-9
Google Scholar
6. Falotico JM, Lapides R, Lipner SR. Combination therapy should be reserved as second-line treatment of onycho- mycosis: a systematic review of onychomycosis clinical trials. J Fungi 2022;8:279
Google Scholar
7. Jerajani HR, Amladi ST, Bongale R, Adepu V, Tendolkar UM, Sentamilselvi G, et al. Evaluation of clinical efficacy and safety of once daily topical administration of 1% oxiconazole cream and lotion in dermatophytosis: an open label, non comparative multicentre study. Indian J Dermatol Venereol Leprol 2000;66:188-192
Google Scholar
8. Carney C, Tosti A, Daniel R, Scher R, Rich P, DeCoster J, et al. A new classification system for grading the severity of onychomycosis: Onychomycosis Severity Index. Arch Dermatol 2011;147:1277-1282
Google Scholar
9. Lim SS, Ohn JY, Mun JH. Diagnosis of onychomycosis: from conventional techniques and dermoscopy to artificial intelligence. Front Med (Lausanne) 2021;8:637216
Google Scholar
10. Park J, Nam JH, Lee JH, Park JS, Mun JH, Lee YW, et al. Korean guideline for the diagnosis and treatment of onychomycosis: purpose and process of algorithm guide- line development. J Mycol Infect 2018;23:33-44
Google Scholar
11. Gupta AK, Simpson FC. New pharmacotherapy for the treatment of onychomycosis: An update. Expert Opin Pharmacother 2015;16:227-236
12. Xu Y, Miao X, Zhou B, Luo D. Combined oral terbinafine and long-pulsed 1,064-nm Nd:YAG laser treatment is more effective for onychomycosis than either treatment alone. Dermatol Surg 2014;40:1201-1207
Google Scholar
13. Gupta AK, Foley KA, Mays RR, Shear NH, Piguet V. Monotherapy for toenail onychomycosis: A systematic review and network meta-analysis. Br J Dermatol 2020; 182:287-299
Google Scholar
14. Sigurgeirsson B, Ólafsson JH, Steinsson Jþ, Paul C, Billstein S, Evans EG. Long-term effectiveness of treatment with terbinafine vs itraconazole in onychomycosis: A 5-year blinded prospective follow-up study. Arch Dermatol 2002; 138:353-357
15. Park KY, Suh JH, Kim BJ, Kim MN, Hong CK. Randomized clinical trial to evaluate the efficacy and safety of combin- ation therapy with short-pulsed 1,064-nm Neodymium-Doped Yttrium Aluminium Garnet Laser and amorolfine nail lacquer for onychomycosis. Ann Dermatol 2017;29: 699-705
Google Scholar
16. El-Tatawy RA, Abd El-Naby NM, El-Hawary EE, Talaat RA. A comparative clinical and mycological study of Nd-YAG laser versus topical terbinafine in the treatment of onychomycosis. J Dermatolog Treat 2015;26:461-464
Google Scholar
17. Nam JH, Kim JY. Laser and light sources in the treatment of onychomycosis. Korean J Med Mycol 2017;22:87-97
Google Scholar
18. Helou J, Maatouk I, Hajjar MA, Moutran R. Evaluation of Nd:YAG laser device efficacy on onychomycosis: a case series of 30 patients. Mycoses 2016;59:7-11
Google Scholar
19. Gupta AK, Foley KA, Daigle D. Clinical trials of lasers for toenail onychomycosis: The implications of new regu- latory guidance. J Dermatolog Treat 2017;28:264-270
Google Scholar
20. Gupta AK, Venkataraman M, Quinlan EM. Efficacy of lasers for the management of dermatophyte toenail onychomycosis. J Am Podiatr Med Assoc 2022;112:20-236
Google Scholar
21. Ricardo JW, Lipner SR. Safety of current therapies for onychomycosis. Expert Opin Drug Saf 2020;19:1395-1408
Google Scholar
22. Khater MH, Khattab FM. Combined long-pulsed Nd-Yag laser and itraconazole versus itraconazole alone in the treatment of onychomycosis nails. J Dermatolog Treat 2022;31:406-409
Google Scholar
23. Li Y, Xu J, Zhao JY, Zhuo FL. Self-controlled study of onychomycosis treated with long-pulsed Nd:YAG 1,064-nm laser combined with itraconazole. Chin Med J 2016; 129:1929-1934
Google Scholar
24. Xu ZL, Xu J, Zhuo FL, Wang L, Xu W, Xu Y, et al. Effects of laser irradiation on Trichophyton rubrum growth and ultrastructure. Chin Med J 2012;125:3697-3700
Google Scholar
25. Evans EG. The rationale for combination therapy. Br J Dermatol 2001;145:9-13
Congratulatory MessageClick here!