pISSN : 3058-423X eISSN: 3058-4302
Open Access, Peer-reviewed

pISSN : 3058-423X eISSN: 3058-4302
Open Access, Peer-reviewed
Jung Eun Seol,Seong Min Hong,Seung Hee Jang,Sang Woo Ahn,Jong Soo Choi,Jeong Hwan Shin,Jayoung Kim,Hyojin Kim
10.17966/JMI.2022.27.4.85 Epub 2023 January 04
Abstract
Dermatophytes invade the stratum corneum and infect the skin, nails, and hair, mostly resulting in superficial infections. Deep dermatophytosis involving the dermis and subcutaneous layer has rarely been reported in immunocompromised individuals. Herein, we report a case of deep dermatophytosis caused by Trichophyton rubrum. A 71-year-old woman presented with multiple erythematous exophytic and subcutaneous nodules in both the lower legs. The patient was taking immunosuppressive agents for rheumatoid arthritis and antifungal agents for tinea pedis and onychomycosis, which was improperly ceased. Histopathological findings showed diffuse granulomatous infiltration with multinucleated cells, lymphocytes, histiocytes, and neutrophils in the dermis. Septate and branched hyphae were observed in the dermis using periodic acid-Schiff diastase and Gomori methenamine silver staining. T. rubrum was identified in fungal culture from the tissue sample and confirmed through phylogenetic analysis of the internal transcribed spacer and large subunit regions in ribosomal ribonucleic acid gene. Intravenous amphotericin B was administered for septic shock before the confirmation of the causative organism, which rapidly improved the condition.
Keywords
Deep dermatophytosis Trichophyton rubrum
Dermatophytes are the most common cause of superficial fungal infections in humans; Trichophyton (T.) rubrum is the most frequently isolated pathogen1. In humans, dermato- phytes are mainly confined to the stratum corneum, nails, and hair. Dermatophytes do not actively penetrate deeper than the basal layer2. They rarely penetrate deeply into the dermis and cause invasive infections involving hair follicles; the dermis; subcutaneous tissue; and even internal organs, such as the lymph nodes, bone, and brain1. Invasive dermato- phytosis is typically associated with immunosuppression and lymphoproliferative disorders. Compared with immunocom- petent patients, patients with immunosuppression have an increased risk of invasive form transformation, owing to chronic infection resulting from a higher rate of recurrence and recalcitrance. Herein, we report an atypical presentation of deep dermatophytosis as multiple exophytic masses in the bilateral lower limbs.
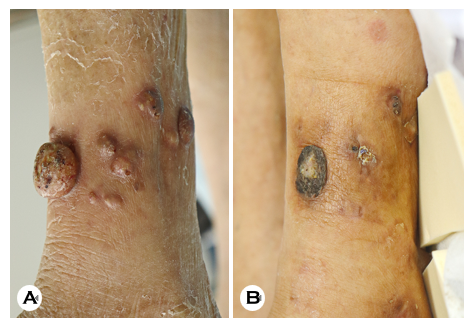
A 71-year-old woman admitted for pneumonia was referred for an erythematous exophytic mass with multiple subcuta- neous nodules on both lower legs (Fig. 1A). The initial skin lesion was detected on the left leg a month before referral, which subsequently spread to the adjacent tissue and the right leg. The patient had a history of rheumatoid arthritis and was treated immunosuppressants, such as tacrolimus, low-dose systemic steroid, leflunomide, and methotrexate, for more than 10 years. Furthermore, she had taken an antifungal medication for tinea pedis and unguium; however, she decided to discontinue the treatment.
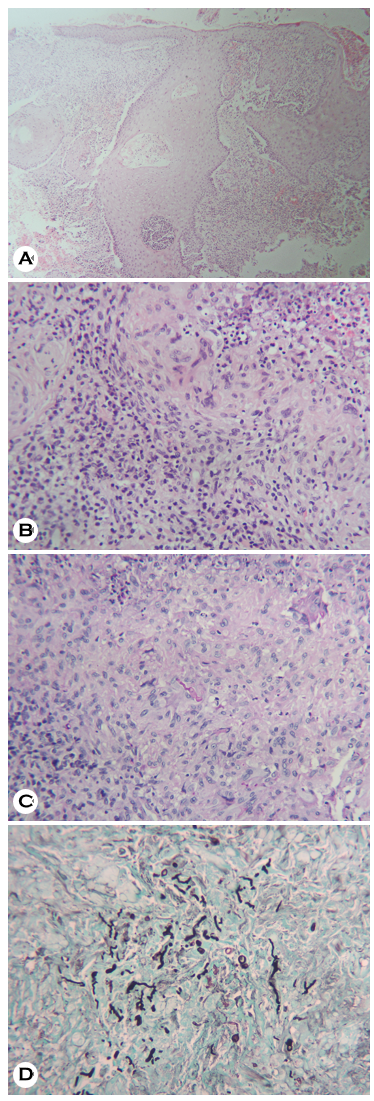
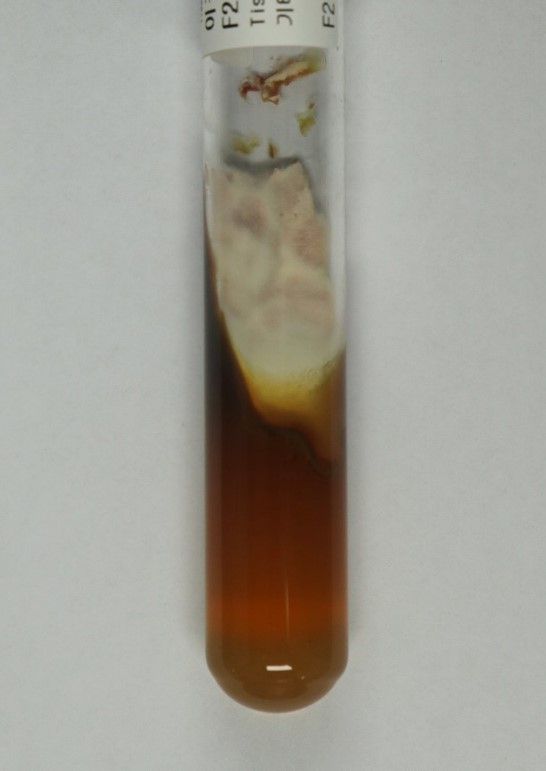
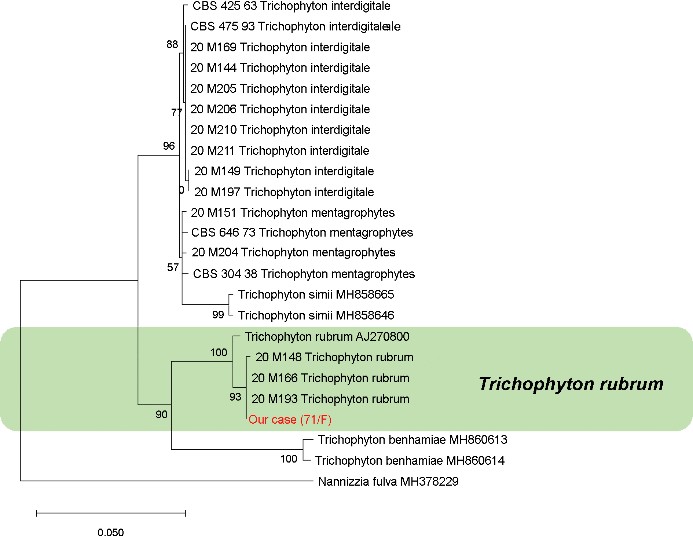
A deep fungal infection was suspected based on her skin lesion and history. A skin biopsy was performed on her left lower leg. Histopathological examination revealed pseudo- epitheliomatous epidermal hyperplasia with micro-abscess formation in the epidermis and diffuse granulomatous inflam- mation consisting of multinucleated giant cells, lymphocytes, neutrophils, and histiocytes in the dermis. Immunohisto- chemical staining with periodic acid-Schiff and Gomori methe- namine silver revealed septate and branched fungal hyphae in the dermis (Fig. 2). Fungal cultures performed using biopsy tissue showed red-brown pigmentation, suggesting Tricho- phyton species infection (Fig. 3). A molecular approach was used based on the sequence analysis of ribosomal DNA (rDNA). T. rubrum was identified by phylogenetic analysis using internal transcribed spacer and large subunit (LSU) region sequencing of ribosomal RNA gene (Fig. 4).
Before the identification of the causative organism, the patient's condition deteriorated because of septic shock. Amphotericin B was administered empirically for 6 days to prevent hematogenous dissemination, and the skin lesions resolved simultaneously (Fig. 1B).
Dermatophytes cause superficial infections of the skin and rarely cause deep infections invading the dermis in patients with acquired or innate immunosuppression. Most patients acquired immunosuppression are organ transplant recipients. However, it can occur in patients receiving immunosup- pressive treatments for other diseases, such as interstitial lung disease3 and rheumatoid arthritis, as observed in our case4. Recently, deep dermatophytosis has been reported in healthy individuals with a genetic predisposition to fungal organisms, such as those with autosomal recessive caspase recruitment domain-containing protein 9 (CARD9) deficiency5 and C282Y mutation6. According to a recent systematic review, the most common predisposing factor for invasive dermatophytosis is superficial dermatophytosis, followed by solid organ trans- plantation, topical immunosuppressant use, gene mutation, diabetes mellitus, and trauma1. Deep dermatophytosis is classi- fied into three types: (i) Majocchi granuloma, (ii) deeper dermal dermatophytosis, and (iii) disseminated dermatophytosis6. This case corresponded to deeper dermal dermatophytosis. In contrast to Majocchi granulomas, it is characterized by a rapidly growing lesion, commonly confined to the extremities without the involvement of other internal organs. Although the mechanism of fungal invasion in the dermis is yet to be clarified, the possibility of follicular invasion7,8 or direct invasion from the epidermis into the dermis has been raised3,9. In most cases of deep dermatophytosis, T. rubrum is the most common causative agent; however, other species, such as T. violaceum, T. mentagrophytes, T. verrucosum, and T. ferru- gineum, have also been found1,7. There is no established treatment for deep dermatophytosis; however, systemic anti- fungal drugs, such as terbinafine, itraconazole, and griseo- fulvin, are usually used. Although the treatment duration differs depending on each patient's immune status, most patients respond well to systemic antifungal drugs. In a recent study, terbinafine was recommended as the first-line treatment for immunocompromised patients as its administration is safer than azole drugs10. However, as resistance to antifungal drugs has increased recently, identifying the causative fungal patho- gen is crucial. Combined treatment with multiple antifungal agents should be considered when genetic abnormalities, such as CARD9 deficiency, are present1. In this case report, before the pathogen was identified, the patient's systemic condition deteriorated rapidly. Therefore, systemic antibiotics and amphotericin B were simultaneously administered, and the skin lesions improved. Deep dermatophytosis can easily be mistaken for another disease, as it appears in various clinical manifestations. If treatment is delayed, immunocompetent patients can progress to a severe disease course, such as hematogenous dissemination. Hence, clinicians should differ- entiate this disease and conduct treatment at an appropriate time. Herein, we report a case of deep dermatophytosis in an immunocompromised patient who was successfully treated with amphotericin B.
References
1. Wang R, Huang C, Zhang Y, Li R. Invasive dermatophyte infection: A systematic review. Mycoses 2021;64:340-348
Google Scholar
2. Toussaint F, Sticherling M. Multiple dermal abscesses by Trichophyton rubrum in an immunocompromised patient. Front Med (Lausanne) 2019;6:97
Google Scholar
3. Demidovich CW, Kornfeld BW, Gentry RH, Fitzpatrick JE. Deep dermatophyte infection with chronic draining nodules in an immunocompromised patient. Cutis 1995; 55:237-240
Google Scholar
4. Blank H, Smith JG Jr. Widespread Trichophyton rubrum granulomas treated with griseofulvin. Arch Dermatol 1960;81:779-789
Google Scholar
5. Lanternier F, Pathan S, Vincent QB, Liu L, Cypowyj S, Prando C, et al. Deep dermatophytosis and inherited CARD9 deficiency. N Engl J Med 2013;369:1704-1714
Google Scholar
6. Marconi VC, Kradin R, Marty FM, Hospenthal DR, Kotton CN. Disseminated dermatophytosis in a patient with hereditary hemochromatosis and hepatic cirrhosis: case report and review of the literature. Med Mycol 2010;48: 518-527
Google Scholar
7. Inaoki M, Nishijima C, Miyake M, Asaka T, Hasegawa Y, Anzawa K, et al. Case of dermatophyte abscess caused by Trichophyton rubrum: a case report and review of the literature. Mycoses 2015;58:318-323
Google Scholar
8. Baker RL, Para MF. Successful use of ketoconazole for invasive cutaneous Trichophyton rubrum infection. Arch Intern Med 1984;144:615-617
Google Scholar
9. Grossman ME, Pappert AS, Garzon MC, Silvers DN. Invasive Trichophyton rubrum infection in the immuno- compromised host: report of three cases. J Am Acad Dermatol 1995;33:315-318
Google Scholar
10. Rouzaud C, Chosidow O, Brocard A, Fraitag S, Scemla A, Anglicheau D, et al. Severe dermatophytosis in solid organ transplant recipients: a French retrospective series and literature review. Transpl Infect Dis 2018;20:e12799
Google Scholar
Congratulatory MessageClick here!