pISSN : 3058-423X eISSN: 3058-4302
Open Access, Peer-reviewed

pISSN : 3058-423X eISSN: 3058-4302
Open Access, Peer-reviewed
Su Min Lee,Sook Jung Yun,Jee-Bum Lee
10.17966/JMI.2022.27.4.82 Epub 2023 January 04
Abstract
Leukonychia is the white discoloration of the nail, and it is a common chromatic abnormality of the nail. Leukonychia can be caused by various systemic conditions; however, a fungal infection is also a probable cause. Herein, we report two cases that presented with varying patterns of single-nail leukonychia and were diagnosed with fungal leukonychia based on potassium hydroxide (KOH) examination and fungal culture. A 59-year-old man presented with asymptomatic complete whitish discoloration of the right fourth fingernail. KOH examination revealed many septate hyphae, and Trichophyton rubrum was identified through fungal culture and 18S rRNA sequencing. A 32-year-old man presented with asymptomatic longitudinal ridges and pitting with partial whitish discoloration of the second left fingernail persistent for 5 years. KOH examination revealed many short hyphae, and Scedosporium species was identified on fungal culture.
Keywords
Finger nail Fungal leukonychia Scedosporium Trichophyton rubrum
Leukonychia is a common abnormality of the nail with diverse etymologies, such as systemic diseases, hereditary causes, and dermatological conditions. Fungal infections are a possible cause of leukonychia; particularly, superficial white onychomycosis and primary subungual onychomycosis can make the nails white1. Fungal leukonychia usually affects the toenails, and in cases where fingernails are affected, con- current toenail onychomycosis typically occurs2. We report two cases of single-fingernail leukonychia without toenail infections and other fingernail changes.
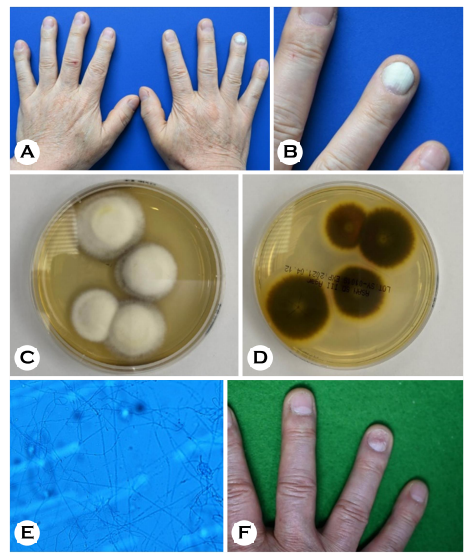
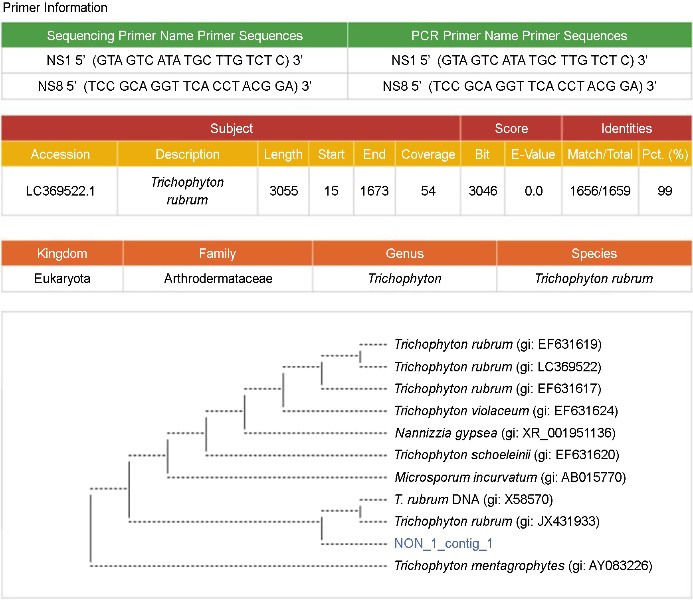
A 59-year-old man with a history of pemphigus vulgaris presented with asymptomatic total whitish discoloration of the fourth right fingernail, the onset of which was several months ago (Fig. 1A, B). Except for the fourth nail on the right hand, no other fingernails or toenails were affected. This patient was receiving daily low-dose systemic steroids (5~10 mg methylprednisolone daily) since 2017 for pemphigus vulgaris. The patient's medical history was unremarkable for any treatment for fingernail abnormalities. To confirm onycho- mycosis, a nail potassium hydroxide (KOH) examination was performed, which revealed several septal mycelia. Fungal culture with subungual debris was performed on a Sabouraud dextrose agar (SDA) with cycloheximide. White fluffy col-onies with a central umbo and a peripheral flat shape were observed from the top view of the SDA plate, and a brownish to wine-red color was observed in the bottom view (Fig. 1C, D). Furthermore, microconidia were observed along the lateral side of the hyphae on lactophenol cotton blue stain (LCBS) (Fig. 1E). Trichophyton rubrum was suspected as the causal organism, and 18S rRNA sequencing revealed Trichophyton rubrum as a significant pathogen (Fig. 2). We grinded the nail surface to allow the drug to permeate well. The nail lesion improved after the application of topical efinaconazole for 3 months (Fig. 1F).
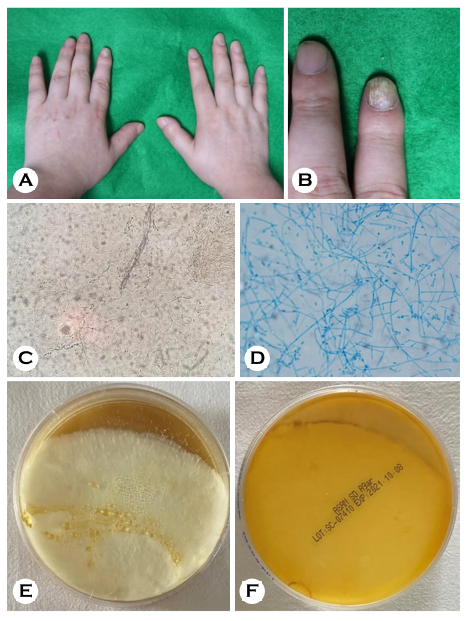
A 32-year-old man presented with asymptomatic longi- tudinal ridges and pitting with partial whitish discoloration on the left second fingernail for 5 years (Fig. 3A, B). The patient's medical history was unremarkable. Although he was treated with oral medication at a private clinic, no improve- ment was observed. The fingernail had fallen out several times. KOH examination revealed several short hyphae (Fig. 3C). White cottony colonies were observed from the top and bottom views of the fungal culture on SDA (Fig. 3E, F). Oval-shaped conidia were observed on LCBS (Fig. 3D). Therefore, the Scedosporium species was identified as a causal organism. After 2 months of oral terbinafine combined with topical efinaconazole treatment, the fingernail lesion improved.
Leukonychia manifests as whitish discoloration of the nail. Its etymology ranges from genetic to acquired, such as fungal infections. Leukonychia can be caused by nail plate or nail bed abnormalities. True leukonychia and pseudo-leukonychia are caused by nail plate abnormalities, and apparent leukonychia, such as Terry's nail, are caused by nail bed abnormalities. Among fungal infections, proximal subungual onychomycosis and white superficial onychomycosis cause leukonychia, both of which originate from nail plate abnormalities1.
The clinical features of the two patients were white super- ficial onychomycosis, in which they showed a superficial white patch on the nail plate.
According to Piraccini and Tosti, Trichophyton interdigitale is the most common causal organism in white superficial onychomycosis2. White superficial onychomycosis due to Trichophyton interdigitale always involves the toenails, usually the first one, and presents as 1~5 small whitish opaque friable patches on the nail. Trichophyton rubrum was found to be the cause in four of 79 patients2. In our cases, Trichophyton rubrum was found to be the causal organism in the first patient as well.
In the report by Piraccini and Tosti, 21% of the cases of white superficial onychomycosis were caused by nonder- matophytes2. In the second patient, Scedosporium, a non-dermatophyte, was found to be the causal agent. Although rare, Scedosporium has been reported to be the causal fungus in onychomycosis3.
The involvement of more than one fingernail without a concomitant toenail infection is rare in onychomycosis, unless the patient experienced trauma or is immunosuppressed4.
White superficial onychomycosis typically affects ≥1 toenails, most commonly the first, second, and third toenails. The involvement of the fingernails in adults has rarely been de- scribed5.
In our cases, the first patient was on prolonged systemic steroid treatment after the diagnosis of pemphigus. Although the second patient had no history of trauma, he complained of frequent nail loss. Both patients showed the involvement of only one fingernail, and these cases were uncommon, in whom no other nails were affected.
In summary, both patients showed leukonychia on one nail without the involvement of any other nails, although the cause was a fungal infection. Our report suggests that fungal causes should be suspected in leukonychia of the nail, and KOH examination and fungal culture should be performed for an accurate diagnosis.
References
1. Grossman M, Scher RK. Leukonychia. Review and classifi- cation. Int J Dermatol 1990;29:535-541
Google Scholar
2. Piraccini BM, Tosti A. White superficial onychomycosis: epidemiological, clinical, and pathological study of 79 patients. Arch Dermatol 2004;140:696-701
Google Scholar
3. Issakainen J, Heikkilä H, Vainio E, Koukila-Kähkölä P, Castren M, Liimatainen O, et al. Occurrence of Scopula- riopsis and Scedosporium in nails and keratinous skin. A 5-year retrospective multi-center study. Med Mycol 2007; 45:201-209
Google Scholar
4. Gupta AK, Stec N, Summerbell RC, Shear NH, Piguet V, Tosti A, et al. Onychomycosis: a review. J Eur Acad Dermatol Venereol 2020;34:1972-1990
Google Scholar
5. Kornbleuth S, Hsu S. White superficial onychomycosis of the fingernail caused by Trichophyton rubrum in an immunocompetent patient. Cutis 1999;64:99-100
Google Scholar
Congratulatory MessageClick here!