pISSN : 3058-423X eISSN: 3058-4302
Open Access, Peer-reviewed

pISSN : 3058-423X eISSN: 3058-4302
Open Access, Peer-reviewed
Joon Ho Son,Yeong Ho Kim,Ji Hyun Lee
10.17966/JMI.2021.26.4.95 Epub 2022 January 01
Abstract
The patient provided written informed consent for the publication and the use of his images.
Keywords
Balanoposthitis Candida albicans Coinfection Lactobacillus spp.
Balanoposthitis is an inflammation affecting both the glans penis and prepuce1. It occurs in approximately 3~11% of males1,2. Nonspecific balanoposthitis commonly results from poor hygiene1. In cases of balanoposthitis caused by infections due to unhygienic circumstances, appropriate treatment of the underlying pathogen is required1,3. Therefore, it is essential to identify the causative factors.
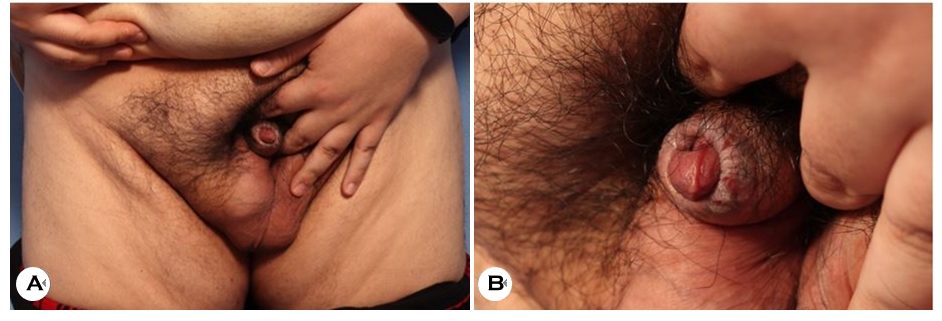
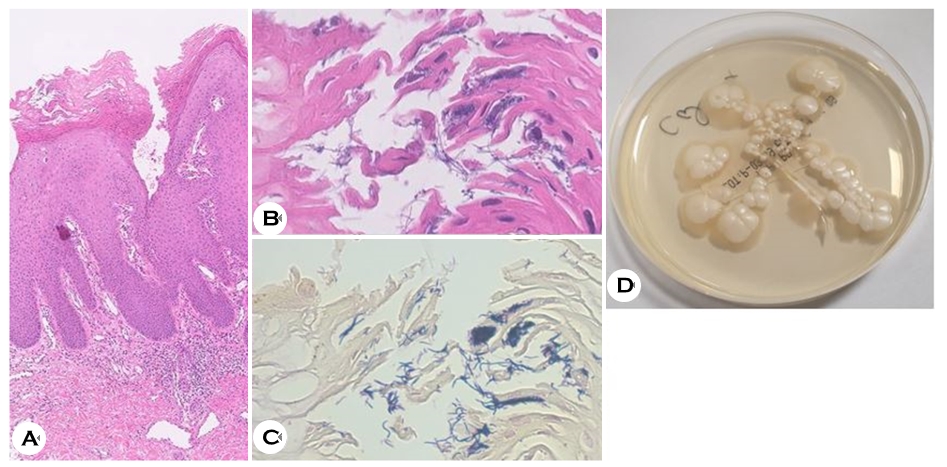
A 31-year-old male presented with a painful, itchy, erythematous-to-whitish, erosive patch on the prepuce of the penis, which had persisted for 1 year. Before the clinical visit, the patient had been treated with oral antibiotics and anti- fungals, including isoconazole, topical antifungals, and steroids, but not concurrently. The patient was circumcised, but the symptoms did not improve. He had no underlying medical history but was severely obese with a body mass index of 41.5 kg/m2. Physical examination revealed that the penis was completely buried below the surface of the skin due to the patient's severe obesity, and the erythematous-to-whitish erosive patch on the prepuce was accompanied by erythema on the glans penis, which was suggestive of balanoposthitis (Fig. 1). In addition, the patient's random glucose level was elevated to 230 mg/dl and the urological examination detected glycosuria, suggesting undiagnosed diabetes mellitus. Fungal culture on Sabouraud dextrose agar showed smooth, creamy-white colonies (Fig. 2D) identified as Candida albicans using matrix-assisted laser desorption/ionization time-of-flight mass spectrometry (MALDI-TOF MS). Antifungal susceptibility test was also conducted, which showed susceptibility to fluco- nazole. Bacterial culture demonstrated growth of Lactobacillus spp. and Staphylococcus epidermidis. Skin biopsy showed parakeratotic hyperkeratosis and epidermal acanthosis, with a mild perivascular lymphohistiocytic infiltration in the upper dermis (Fig. 2A), and gram-positive, basophilic rod-shaped bacteria in the stratum corneum (Fig. 2B, 2C). The patient was treated with oral doxycycline (200 mg/day), fluconazole (150 mg once a week), topical fluconazole (in the morning), isoconazole cream (in the evening), and ofloxacin ointment (twice a day) for 4 weeks. After treatment, the lesion and symptoms improved significantly.
Balanoposthitis has a wide variety of causes and predisposing factors, most commonly diabetes1,2. Balanoposthitis in patients with diabetes are usually infectious4. The most common pathogen is Candida albicans, and other causes of infection include aerobic bacteria, such as Staphylococcus aureus, Group A Streptococcus, anaerobic bacteria, and herpes simplex virus4. Glycemic control in patients with diabetes is important since glycosuria increases the growth of the pathogenic microorganisms4. Obesity can cause chronic irritation, poor genital hygiene, and improper immune re- sponses, thus increasing the risk for balanoposthitis5. Balanoposthitis can involve various factors; hence, the importance of determining the underlying pathogen and predisposition of the patient is essential for appropriate treatment.
This case emphasizes the importance of bacterial and fungal cultures for the appropriate treatment of the underlying pathogen(s) in patients with balanoposthitis, due to possible coninfections with multiple pathogens. Glycemic control and weight loss are crucial for patients with chronic or recurrent balanoposthitis, uncontrolled diabetes, and obesity.
References
1. Edwards S. Balanitis and balanoposthitis: a review. Genitourin Med 1996;72:155-159
Google Scholar
2. Vohra S, Badlani G. Balanitis and balanoposthitis. Urol Clin North Am 1992;19:143-147
Google Scholar
3. Edwards SK. European Branch of the International Union against Sexually Transmitted Infection and the European Office of the World Health Organization. European guideline for the management of balanoposthitis. Int J STD & AIDS 2001;12(Suppl 3):68-72
Google Scholar
4. Kalra S, Chawla A. Diabetes and balanoposthitis. J Pak Med Assoc 2016;66:1039-1041
Google Scholar
5. Fuchs ME, Beecroft N, Dajusta DG, McLeod DJ. The asso- ciation between BXO and obesity in boys undergoing circumcision. Glob Pediatr Health 2017;4:2333794X-17742749
Google Scholar
Congratulatory MessageClick here!