pISSN : 3058-423X eISSN: 3058-4302
Open Access, Peer-reviewed

pISSN : 3058-423X eISSN: 3058-4302
Open Access, Peer-reviewed
Kyung Duck Park,Eun Hye Lee,Seon Hwa Lee,Yong Jun Bang,Jae Bok Jun,Jong Soo Choi,Dae-Lyong Ha,Jun Young Kim,Yong Hyun Jang,Seok-Jong Lee,Weon Ju Lee
10.17966/JMI.2021.26.2.45 Epub 2021 July 01
Abstract
Keywords
Chromoblastomycosis is a chronic granulomatous or ver- rucous skin condition that is mainly caused by Fonsecaea pedrosoi, Phialophora verrucose, and Cladophialophora carrionii . The recent taxonomic revision of the genus Fonsecaea has recognized four species: F. pedrosoi, F. monophora, F. nubica, and F. pugnacius. In this case report, we introduce the first case of F. nubica skin infection in Korea.
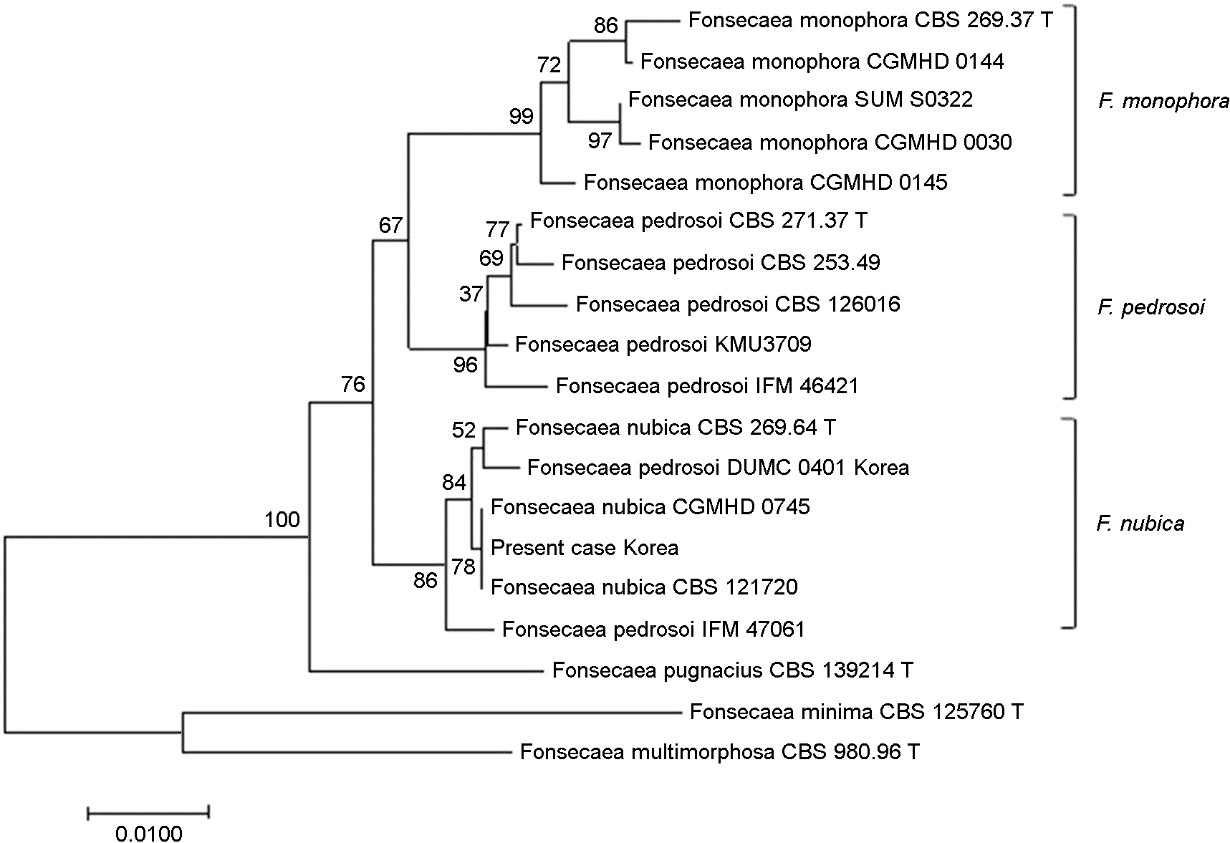
An 84-year-old female visited our clinic with a soft, mica- ceous, scaly plaque surrounded by an erythematous scarring on the left inner wrist and dorsal hand area. The patient could not recall its onset or any history of trauma, but she reported its chronic progression over several years, which was accompanied by a painful or burning sensation. The patient had no significant past history of illnesses. The KOH examination of the wrist lesion showed sclerotic cells. The fungal culture showed a black-gray velvety colony (Fig. 1A) with Cladosporium-type conidia (Fig. 1B). The skin biopsy obtained from the granulation tissue showed aggregated neutrophil infiltration and lymphohistiocytes on the perivascular area of the dermis. Sclerotic cells were identified in this area (Fig. 1C). The evaluation of homology was done using the Basic Local Alignment Search Tool on the GenBank database. The internal transcribed spacer (ITS) region of ribosomal DNA was identified as F. nubica (used primers were ITS1 and ITS4). Gene sequencing revealed 100% homology with strain CBS 121720 and CGMHD 0745. Identity with other Fonsecaea species were 97.55% with F. pedrosoi type strain CBS 271.37 and 96.30% with F. monophora type strain CBS 269.37 (Fig. 2). The patient was treated with 100 mg itraconazole taken orally twice a day. After nine months, three coin-sized, wart-like, granulomatous plaque lesions remained (Fig. 1D), and local cryotherapy was also applied. Two months after the combination treatment, the patient demonstrated a good clinical improvement.
Although the four Fonsecaea species have similar morpho- logies, they have different pathogenicity. F. pedrosoi and F. nubica appear to be exclusively associated with chromo- blastomycosis, whereas F. monophora was found to cause chromoblastomycosis and infections in other organs, including the brain, gallbladder, and lymph nodes. The presence of muriform cells (Medlar bodies or sclerotic cells) and the identification of an etiological agent in a microbiological culture are necessary to confirm the diagnosis of chromoblasto- mycosis. Fonsecaea species are often misidentified due to their indistinct morphological features. Moreover, the re- classification of the genus Fonsecaea is being made by molecular genetics. For strain DUMC 0401, it was reported as F. pedrosoi in 2010 by Lim SW et al.; its ITS sequence was 99.47% identical with that of the present case. Based on the results of the phylogenetic analysis, this strain should be reclassified as F. nubica (Fig. 2). It is possible that there had been previous unreported cases of chromoblastomycosis caused by F. nubica in Korea. The treatment of chromoblastomycosis is challenging as there is currently no treatment of choice. Many modalities, including systemic antifungal agents, immunomodulatory therapy, physical methods, photodynamic therapy, and surgical excision, have been used in previous reports. Itraconazole is the most commonly used first-line agent. A successful treatment with voriconazole or posaconazole has also been described. In this case, we were able to get good results using oral itraconazole, followed by a combination therapy with cryotherapy.
References
1. Krzyściak PM, Pindycka-Piaszczyńska M, Piaszczyński M. Chromoblastomycosis. Postepy Dermatol Alergol 2014; 31:310-321
2. Fransisca C, He Y, Chen Z, Liu H, Xi L. Molecular iden- tification of chromoblastomycosis clinical isolates in Guangdong. Med Mycol 2017;55:851-858.
Google Scholar
3. Queiroz-Telles F, Esterre P, Perez-Blanco M, Vitale RG, Salgado CG, Bonifaz A. Chromoblastomycosis: an over- view of clinical manifestations, diagnosis and treatment. Med Mycol 2009;47:3-15
Google Scholar
4. Lim SW, Suh MK, Kang GS, Ha GY, Kim H, Choi JS, et al. Molecular phylogenetics of Fonsecaea strains isolated from chromoblastomycosis patients in South Korea. Mycoses 2011;54:e415-e420
Google Scholar
5. Yang CS, Chen CB, Lee YY, Yang CH, Chang YC, Chung WH, et al. Chromoblastomycosis in Taiwan: a report of 30 cases and a review of the literature. Med Mycol 2018; 56:395-405
Google Scholar
Congratulatory MessageClick here!