pISSN : 3058-423X eISSN: 3058-4302
Open Access, Peer-reviewed

pISSN : 3058-423X eISSN: 3058-4302
Open Access, Peer-reviewed
Woo Jung Jin,Seong Min Hong,Seung Hee Jang,Hyojin Kim
10.17966/JMI.2022.27.2.43 Epub 2022 July 01
Abstract
Keywords
Cutinebacterium Facial mask Hypopigmention Progressive macular hypomelanosis
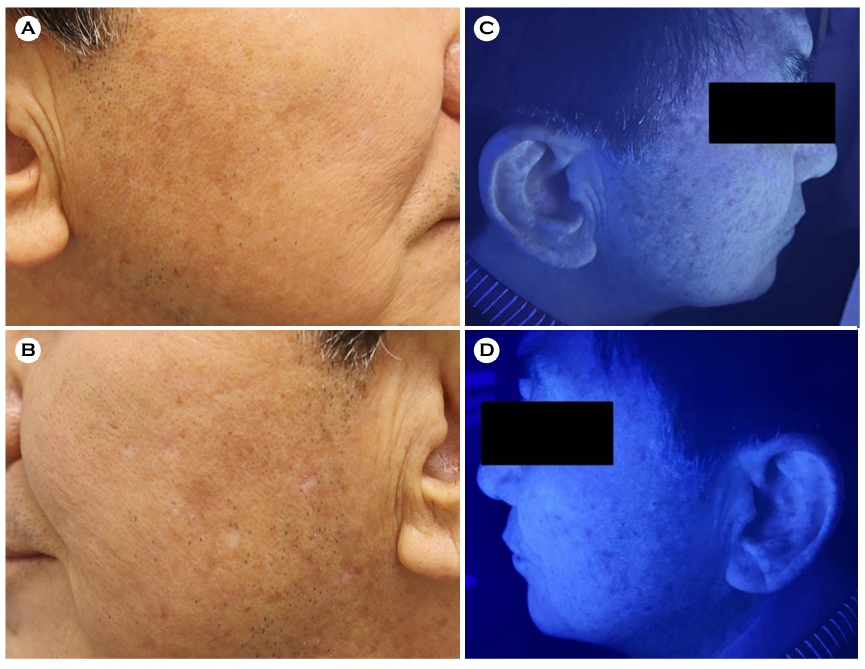
A 61-year-old male patient presented with hyper- and hypo-pigmented finely scaled macules (Fig. 1A, B). He had recently started training at the indoor gym, wearing a facial mask for more than 2 hours a day, during exercise, without replacement. The potassium hydroxide mount of the skin scrapping revealed short hyphae and spores, leading to a provisional diagnosis of tinea versicolor (TV), but topical anti- fungal medications failed to work. Additionally, Wood's lamp examination did not show any characteristics of vitiligo (Fig. 1C, D). Combination treatment with topical tacrolimus and excimer laser was introduced under the suspicion of progressive macular hypomelanosis (PMH) and achieved a partial resolution.
The bacterial community composition of the facial skin was dominated by lipophilic Cutibacterium species, whereas the fungal community by Malassezia1. TV caused by Malassezia usually occurs on the trunk in a warm and humid environment. PMH is commonly seen on the trunk but rarely on the face because of the absence or low abundance of C. acnes type III2.
Continuous use of face masks increases temperature, humidity, and sebum secretion in the covered area3 leading to alterations in the skin microbiome. Thus, the microenviron- ment of the area under the mask appears analogous to the trunk covered with clothing. Furthermore, facial PMH occurs in old age, indicating that the distribution of C. acnes type III could vary with age2.
This study suggests the inclusion of TV and PMH when diagnosing patients for pigmentary changes due to the alterations in the facial skin microenvironment in the era of the COVID-19 pandemic.
References
1. Byrd AL, Belkaid Y, Segre JA. The human skin microbiome. Nat Rev Microbiol 2018;16:143-155
Google Scholar
2. McDowell A, McLaughlin J, Layton AM. Is Cutibacterium (previously Propionibacterium) acnes a potential patho- genic factor in the aetiology of the skin disease progressive macular hypomelanosis? J Eur Acad Dermatol Venereol 2021;35:338-344
Google Scholar
3. Scarano A, Inchingolo F, Lorusso F. Facial skin temperature and discomfort when wearing protective face masks: thermal infrared imaging evaluation and hands moving the mask. Int J Environ Res Public Health 2020;17:4624
Google Scholar
Congratulatory MessageClick here!