pISSN : 3058-423X eISSN: 3058-4302
Open Access, Peer-reviewed

pISSN : 3058-423X eISSN: 3058-4302
Open Access, Peer-reviewed
Jungsoo Lee,Jisang Yun,Kihyuk Shin,Hyunchang Ko,Byungsoo Kim,Moon-Bum Kim,Hoonsoo Kim
10.17966/JMI.2022.27.2.32 Epub 2022 July 01
Abstract
Ungual melanoma is known to be frequently misdiagnosed, and the primary misdiagnosis of ungual melanoma includes onychomycosis. We report a very rare case of onychomycosis concealing ungual melanoma in situ. A 52-year-old male patient presented with a yellow to brown thickened left great toenail that had existed for 10 years. In the front view, Hutchinson's sign which refers periungual extension of brown-black pigmentation from melanonychia was also observed on his hyponychium. First, fungal infection of his toenail was confirmed with positive KOH result. Next, a nail biopsy after nail avulsion was done to assess Breslow depth and to determine surgical margin. And ungual melanoma was diagnosed with immunohistochemical stains. Non-amputative wide local excision with 5 mm surgical margin followed by skin grafting was done Unfortunately in three years ungual melanoma in situ has recurred 2 times and then progressed to invasive malignant melanoma, so he was referred to the Department of plastic surgery for further invasive surgical treatment and regularly monitored to check the recurrence. According to a prior retrospective study, 52% of ungual melanomas were clinically misdiagnosed. Thus, proper diagnosis of ungual melanoma is very important for the patients' better prognosis. It would be important for physicians to examine the nail plate as well as the underneath structures for patients with nail disease including onychomycosis.
Keywords
Nail diseases Onychomycosis Subungual melanoma
Onychomycosis, caused by a fungal infection of the nail plate, is the most common nail disorder affecting up to 10% of the general population1. On the other hand, ungual melanoma, a rare subtype of malignant melanoma which arises from structures within the nail unit2 accounts for 3% to 15% of all cutaneous malignant melanomas. The age-standardized incidence of malignant melanomas in Korea is only 0.4 to 0.6 per 100,000 people, which supports the disease's rarity3. Unfortunately, ungual melanoma is frequently misdiagnosed4 sometimes as onychomycosis5. This correct diagnosis delay in the rare case of ungual melanoma may account for the associated relatively poor prognosis6. Here, we report a very rare case of ungual melanoma concealed by onychomycosis.
A 52-year-old male patient with a history of liver cirrhosis presented with a yellow to brown thickened left great toenail that had existed for 10 years. Initially, he had regarded it only as a toenail fungal infection to which he intermittently applied a topical antifungal agent. Nevertheless, proximal nail discoloration began and spread distally a year ago and pigmented macule appeared on the hyponychium of the corresponding toe 3 months ago. A diagnosis of ungual melanoma was made based on histopathologic findings of a skin biopsy of the black macule. The patient was sub- sequently referred to our hospital for further evaluation and management.
Upon examination, his left great toenail exhibited hyper- keratotic yellow to dark brownish discoloration with mild distal nail dystrophy (Fig. 1A). Hutchinson's sign, referring to the periungual extension of brown-black pigmentation from melanonychia, was also observed on the hyponychium (Fig. 1B). Dermoscopy revealed longitudinal melanonychia with yellowish streaks and scales on the nail surface (Fig. 1C).

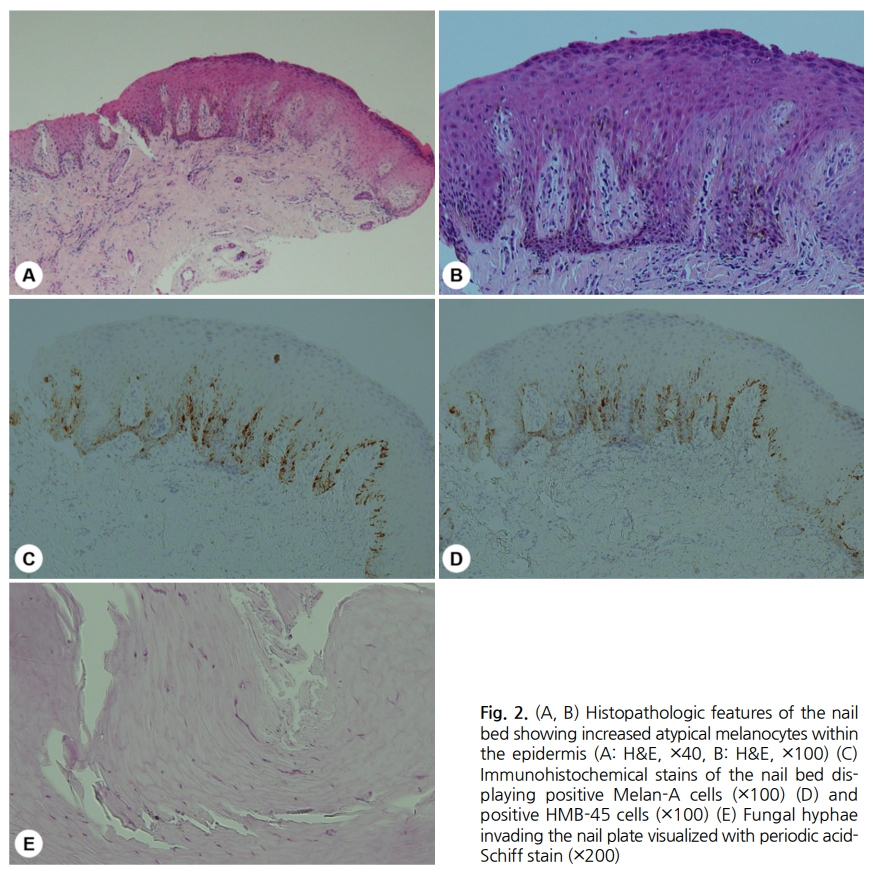
To evaluate and differentiate onychomycosis, a nail potas- sium hydroxide (KOH) test was performed. A positive KOH result confirmed fungal infection of the toenail. Next, since ungual melanoma was diagnosed at a local clinic, a longi- tudinal nail biopsy after nail avulsion was done to assess the Breslow depth and determine the surgical margins. The results revealed increased atypical melanocytes within the epidermis (Fig. 2A, 2B). Immunohistochemical stains of the nail bed displayed Melan-A (Fig. 2C) and HMB-45 (Fig. 2D) positive cells. Furthermore, a periodic acid-Schiff (PAS) stain revealed fungal hyphae invading the nail plate (Fig. 2E). Additional computed tomography scans did not show any evidence of metastasis and laboratory blood tests were within the normal range. Ultimately, a diagnosis was made of onychomycosis with ungual melanoma in situ.
Once the lesion had been histologically confirmed as onycho- mycosis with ungual melanoma in situ, a non-amputative, wide, local excision with a 5-mm surgical margin followed by skin grafting was performed. Unfortunately, over 3 years ungual melanoma in situ recurred twice and progressed to invasive malignant melanoma with a 4-mm depth of invasion 49 months after the first surgery. The patient was subse- quently referred to the department of plastic surgery for distal phalanx amputation and is being closely and regularly monitored to check for recurrence at 6-month intervals. There have been no recurrences or metastasis 25 months after amputation.
Ungual melanoma is an uncommon subtype of malignant melanoma that usually arises from the nail matrix but may also involve other parts of the nail unit, such as the proximal nail fold, nail bed, and hyponychium2. Survival rates for ungual melanoma remain low due to delayed diagnosis when com- pared to other areas of the body including palmoplantar melanomas7,8. Acral melanomas, such as ungual melanomas and palmoplantar melanomas, are often misdiagnosed be- cause they do not typically fit the 'changing mole' pattern8. According to a retrospective study, 52% of ungual mela- nomas were clinically misdiagnosed and were associated with a lower estimated 5-year survival relative to correctly diagnosed lesions (15.4% vs 68.9%)8. Thus, early proper diagnosis of ungual melanoma is very important for a better prognosis.
The two most common misdiagnoses of ungual melanoma are striate melanonychia and onychomycosis. Other incorrect diagnoses include subungual hematoma, junctional nevus, ingrown toenail, and bacterial infection8. In our case, the patient did not recognize the malignant changes of his lesion earlier because of the coexistence of onychomycosis which obscured the traits of ungual melanoma. Thus, he didn't visit a hospital until Hutchinson' sign was present. Ungual melanoma can often be confused with onychomycosis, particularly with fungal melanonychia, since a fungal infection of nails is a much more common condition than ungual melanoma and these diseases share similar clinical pre- sentations such as dark pigmentation and nail dystrophy. Typical clinical features of fungal melanonychia include brown to black pigmentation, sometimes dystrophic, and possible thickening as a result of hyperkeratosis9. On the other hand, ungual melanoma usually displays longitudinal melanonychia with irregular pigmentation, nail dystrophy, and importantly, Hutchinson's sign with long disease duration, age over 50, and a lesion on a great toe10. Hutchinson's sign refers to a periungual extension of brown-black pigmentation from melanonychia11. Although the sign is not pathognomonic and does not always act as an accurate predictor of malignant melanoma, it may suggest the likelihood of ungual melanoma rather than onychomycosis4. Dermoscopy examination helps narrow the differential diagnosis of pigmented nail diseases. Our patient had typical dermoscopic patterns of onycho- mycosis12, showing longitudinal melanonychia with yellowish streaks and scales on the nail surface. There was a limitation of dermoscopic inspection to find the features of ungual melanoma due to hyperkeratotic changes, although dark pigmentation was shown. Hutchinson's sign on the hypony- chium was a clue to check for the coexistence of ungual melanoma. Eventually, the lesion was confirmed by KOH and biopsy of the skin and nail plate and both onychomycosis and ungual melanoma were simultaneously diagnosed. In this case, we assume that the diagnosis of ungual melanoma was delayed due to the presence of onychomycosis which may account for the patient's poor prognosis which pro- gressed to invasive melanoma after two in situ recurrences of ungual melanoma.
This rare case, in which ungual melanoma was masked by onychomycosis, elucidates the importance of thorough in- spection of nail changes, including pigmentation of the nail and skin. Onychomycosis is a very common nail disease, and as shown in this case, it can conceal an underlying nail unit disease. Thus, it is important for physicians to examine the nail plate as well as the underlying structures in patients with nail diseases including onychomycosis.
References
1. Thomas J, Jacobson GA, Narkowicz CK, Peterson GM, Burnet H, Sharpe C. Toenail onychomycosis: an important global disease burden. J Clin Pharm Ther 2010;35:497-519
Google Scholar
2. Tan KB, Moncrieff M, Thompson JF, McCarthy SW, Shaw HM, Quinn MJ, et al. Subungual melanoma: a study of 124 cases highlighting features of early lesions, potential pitfalls in diagnosis, and guidelines for histologic reporting. Am J Surg Pathol 2007;31:1902-1912
Google Scholar
3. Oh CM, Cho H, Won YJ, Kong HJ, Roh YH, Jeong KH, et al. Nationwide trends in the incidence of melanoma and non-melanoma skin cancers from 1999 to 2014 in South Korea. Cancer Res Treat 2018;50:729-737
Google Scholar
4. Levit EK, Kagen MH, Scher RK, Grossman M, Altman E. The ABC rule for clinical detection of subungual mela- noma. J Am Acad Dermatol 2000;42:269-274
Google Scholar
5. Soon SL, Solomon AR Jr, Papadopoulos D, Murray DR, McAlpine B, Washington CV. Acral lentiginous melanoma mimicking benign disease: The Emory experience. J Am Acad Dermatol 2003;48:183-188
Google Scholar
6. Patterson RH, Helwig EB. Subungual malignant melanoma: a clinical-pathologic study. Cancer 1980;46:2074-2087
Google Scholar
7. Patel GA, Ragi G, Krysicki J, Schwartz RA. Subungual melanoma: a deceptive disorder. Acta Dermatovenerol Croat 2008;16:236-242
Google Scholar
8. Metzger S, Ellwanger U, Stroebel W, Schiebel U, Rassner G, Fierlbeck G. Extent and consequences of physician delay in the diagnosis of acral melanoma. Melanoma Res 1998;8:181-186
Google Scholar
9. Finch J, Arenas R, Baran R. Fungal melanonychia. J Am Acad Dermatol 2012;66:830-841
Google Scholar
10. Braun RP, Baran R, Le Gal FA, Dalle S, Ronger S, Pandolfi R, et al. Diagnosis and management of nail pigmentations. J Am Acad Dermatol 2007;56:835-847
Google Scholar
11. Baran R, Kechijan P. Hutchinson's sign: A reappraisal. J Am Acad Dermatol 1996;34:87-90
Google Scholar
12. Kim HJ, Kim TW, Park SM, Lee HJ, Kim GW, Kim HS, et al. Clinical and dermoscopic features of fungal melanonychia: differentiating from subungual melanoma. Ann Dermatol 2020;32:460-465
Google Scholar
Congratulatory MessageClick here!