pISSN : 3058-423X eISSN: 3058-4302
Open Access, Peer-reviewed

pISSN : 3058-423X eISSN: 3058-4302
Open Access, Peer-reviewed
Yu-Mi Lee,Sung-Yeon Cho,Ki-Ho Park,Mi Suk Lee,Young Jin Kim
10.17966/JMI.2020.25.4.71 Epub 2021 January 06
Abstract
No cases of human infections caused by Cladosporium velox have been reported. A 69-year-old female patient with rheumatoid arthritis developed pneumonia with empyema. The fungal cultures of pleural fluid were obtained. Cladosporium was grown from the pleural fluid. C. velox was identified by internal transcribed spacer sequencing. The pathologic results of biopsied lung tissue indicated the presence of fungal hyphae. C. velox can cause clinical infection in an immunocompromised setting.
Keywords
Cladosporium velox Empyema Pneumonia Rheumatoid arthritis
Cladosporium species are rare fungal pathogens involved in clinical infection. Here, we report on a patient with rheu- matoid arthritis who developed pneumonia with empyema caused by Cladosporium velox, which was identified by in- ternal transcribed spacer sequencing. This is the first reported human infection with C. velox.
A 69-year-old female patient with seropositive rheumatoid arthritis, presented with cough and yellowish sputum, was admitted to the Rheumatology Department of Kyung Hee University Hospital in South Korea. The patient had been taking medications including systemic steroids for osteoarthritis for 20 years. She was diagnosed with seropositive rheumatoid arthritis 5 months before being admitted at our institution. For the previous months, the patient was treated with metho- trexate, mizoribine (150 mg daily), and celecoxib for rheu- matoid arthritis. The initial vital signs were within the normal range. Chest computed tomography (CT) scan showed two cavitary lesions, which were 4 and 2 cm in size, in the left upper lung and a 4-cm cavitary lesion in the left lower lung (Fig. 1A). CT-guided core needle biopsy of a cavitary lung lesion was performed. The pathologic report noted chronic granulomatous inflammation with necrosis. Acid-fast bacilli stain and polymerase chain reaction for Mycobacterium tuber- culosis with the obtained tissue were both negative. No bacterial and fungal pathogens were isolated from the sputum and bronchoalveolar lavage fluid. The patient was prescribed only mizoribine for rheumatoid arthritis and did not develop fever during hospitalization. A chest tube was inserted for drainage of pleural effusion on the left lung field after 45 days of admission. In laboratory examinations, white blood cell count was 5.36 × 109/L (62.6% neutrophil), and the level of C-reactive protein (normal value < 48 nmol/L) was 34.7 nmol/L. Pleural fluid analysis revealed a white blood cell count of 161, 300/μL (neutrophil 96%), and the bacterial culture of pleural fluid was negative. CT-guided biopsy of the left cavitary mass was repeatedly performed. The pathologic results indicated the presence of interstitial fibrosis and chronic inflammation with a focal necrosis containing fungal hyphae at the pulmonary tissue (Fig. 1B and 1C). Cladosporium was identified from three sets of fungal culture of the pleural fluid. Dry, dark, and olivaceous green colonies were grown on Sabouraud dextrose agar at 25℃ after 7 days of incubation. Septate hyphae with a separated, branched, and acropetal chain of spherical conidia was suggestive for Cladosporium (Fig. 1D). A fungal culture of the tissue was negative. She was treated with amphotericin B deoxycholate (0.6 mg/kg per day), vancomycin (1 g per day), and imipenem (2 g per day) for about 5 months. The cavitary mass at the left lung fields improved gradually (Fig. 1E). However, the patient died due to progression of hospital-acquired pneumonia caused by an unknown pathogen 8 months since the first admission.
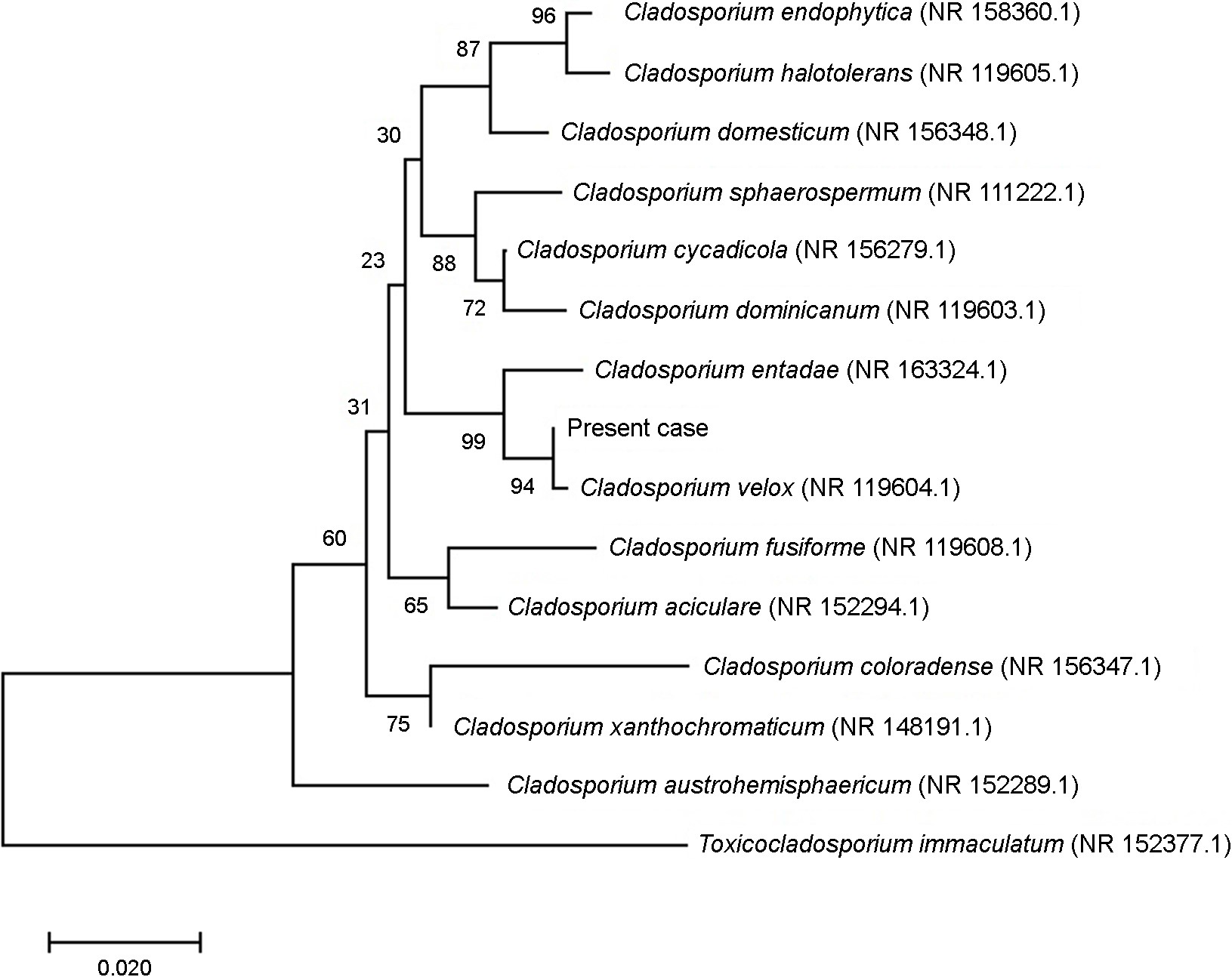
Identification of fungal isolates was assessed via internal transcribed spacer (ITS) sequencing and polymerase chain reaction (PCR) of the β-tubulin gene. In the ITS sequencing of the cultured colony, the best matched taxa obtained using NCBI BLAST against the database for ITS from reference material was C. velox (sequence ID: NR119604.1) with a similarity of 100% (478/478). The second highest match was Cladosporium entadae (Sequence ID: NR_163324.1) with a similarity of 98.4% (479/487). The neighbor-joining tree by MEGA-X, based on ITS, showed C. velox as the nearest taxa (Fig. 2). Antifungal susceptibilities were determined using the broth dilution method. The minimal inhibitory concentrations (MICs) of each antifungal agent were as follows: 2.0 mg/L for voriconazole, 0.5 mg/L for itraconazole, 64 mg/L for fluconazole, 0.5 mg/L for posaconazole, and 1.0 mg/L for amphotericin B deoxycholate. The real-time PCR of formalin-fixed paraffin-embedded (FFPE) lung tissue containing fungal hyphae was performed using the LC480 (Roche Diagnostics, Mannheim, Germany) with primers recognizing benA and ITS, subsequently followed by melting curve analysis. However, fungal isolate was not amplified by tissue real-time PCR. This study was approved by the institutional review board (KHUH 2020-04-028), and it was conducted in compliance with the principles of the Declaration of Helsinki.
Cladosporium are ubiquitous and frequently isolated from environmental sources worldwide. The genus Cladosporium has undergone extensive revisions by polyphasic approaches. The number of species under Cladosporium has increased up to 218 due to continuous isolation from clinical samples and environment. Cladosporium species are often isolated from the respiratory tract and superficial/deep tissue infection. Transmission of Cladosporium are usually via the airborne route because of their small conidia and tendency to detach.
Multilocus gene analysis of the ITS, D1/D2, EF-1α, and actin gene is useful for accurate identification of Cladosporium. The analysis of EF-1α and actin genes identify a high degree of divergence among species, while ITS shows a poor species resolution. However, C. velox in this case was successfully differentiated from other Cladosporium by ITS gene analysis. PCR amplification of β-tubulin gene from the tissue samples was attempted, but the result was not successful. This may be due to problems with DNA extraction and the amount/ length of DNA for PCR from FFPE tissue.
Cladosporium may cause clinically important infections in immunocompromised hosts, albeit rarely. Deep tissue infection, lymphadenitis, mycotic aneurysm, keratitis, pneumonia, meningitis, brain abscess, and pulmonary fungal ball caused by Cladosporium have been reported previously. Notably, no evidence of human infections caused by C. velox had been reported. To our knowledge, this is the first study to report pneumonia and empyema due to C. velox infection. C. velox was the most likely pathogen, as the patient improved with antifungal therapy.
The antifungal susceptibilities of Cladosporium showed variability according to the species. Overall, amphotericin B, terbinafine, micafungin, anidulafungin, itraconazole, and posaconazole exhibit good antifungal activity against Clados- porium, while flucytosine, caspofungin, and voriconazole showed variable in vitro activity. The case patient received amphotericin B deoxycholate (MIC = 1.0 mg/L) for pneumonia /empyema due to C. velox, resulting in a gradual improvement in cavitary pneumonia with empyema. In our case, the patient with rheumatoid arthritis has been prescribed only mizoribine during hospitalization. Mizoribine is a strong immunosup- pressive drug, interrupting DNA synthesis. The rheumatoid arthritis itself combined with the strong immunosuppressive effect of mizoribine may have influenced the response to antifungal therapy for pneumonia/empyema caused by C. velox and affected the development of hospital-acquired bacterial pneumonia.
We present here a case of pneumonia and empyema caused by C. velox in a female patient with rheumatoid arthritis. It is significant to report this case of human infection due to C. velox. Cladosporium may cause clinically important infections in immunocompromised hosts.
References
1. Glass NL, Donaldson GC. Development of primer sets designed for use with the PCR to amplify conserved genes from filamentous ascomycetes. Appl Environ Microbiol 1995;61:1323-1330
Google Scholar
2. Kumar S, Stecher G, Li M, Knyaz C, Tamura K. MEGA X: Molecular evolutionary genetics analysis across computing platforms. Mol Biol Evol 2018;35:1547-1549
Google Scholar
3. Bensch K, Groenewald JZ, Meijer M, Dijksterhuis J, Jurjevic Z, Andersen B, et al. Cladosporium species in indoor environments. Stud Mycol 2018;89:177-301
Google Scholar
4. Bensch K, Braun U, Groenewald JZ, Crous PW. The genus Cladosporium. Stud Mycol 2012;72:1-401
Google Scholar
5. Marin-Felix Y, Groenewald JZ, Cai L, Chen Q, Marincowitz S, Barnes I, et al. Genera of phytopathogenic fungi: GOPHY 1. Stud Mycol 2017;86:99-216
Google Scholar
6. Horner WE, Worthan AG, Morey PR. Air- and dustborne mycoflora in houses free of water damage and fungal growth. Appl Environ Microbiol 2004;70:6394-6400
Google Scholar
7. Voigt K, Wöstemeyer J. Phylogeny and origin of 82 zygomycetes from all 54 genera of the Mucorales and Mortierellales based on combined analysis of actin and translation elongation factor EF-1alpha genes. Gene 2001; 270:113-120
Google Scholar
8. Zalar P, de Hoog GS, Schroers HJ, Crous PW, Groenewald JZ, Gunde-Cimerman N. Phylogeny and ecology of the ubiquitous saprobe Cladosporium sphaerospermum, with descriptions of seven new species from hypersaline environments. Stud Mycol 2007;58:157-183
Google Scholar
9. Jayasinghe RD, Abeysinghe W, Jayasekara PI, Mohomed YS, Siriwardena B. Unilateral cervical lymphadenopathy due to Cladosporium oxysporum: A case report and review of the literature. Case Rep Pathol 2017;2017: 5036514
Google Scholar
10. Sunagawa K, Uchino Y, Ishimoto S, Nakamura S, Honma T, Nakanishi Y, et al. Mycotic pseudoaneurysm of a pulmonary artery branch caused by Cladosporium. Pathol Int 2018;68:47-52
Google Scholar
11. Batra N, Kaur H, Mohindra S, Singh S, Shamanth AS, Rudramurthy SM. Cladosporium sphaerospermum causing brain abscess, a saprophyte turning pathogen: Case and review of published reports. J Mycol Med 2019;29:180 -184
Google Scholar
12. Kwon-Chung KJ, Schwartz IS, Rybak BJ. A pulmonary fungus ball produced by Cladosporium cladosporioides. Am J Clin Pathol 1975;64:564-568
Google Scholar
13. Sandoval-Denis M, Sutton DA, Martin-Vicente A, Cano-Lira JF, Wiederhold N, Guarro J, et al. Cladosporium Species Recovered from Clinical Samples in the United States. J Clin Microbiol 2015;53:2990-3000
Google Scholar
14. Yokota S. Mizoribine: mode of action and effects in clinical use. Pediatr Int 2002;44:196-198
Google Scholar
Congratulatory MessageClick here!