pISSN : 3058-423X eISSN: 3058-4302
Open Access, Peer-reviewed

pISSN : 3058-423X eISSN: 3058-4302
Open Access, Peer-reviewed
Mingyu Kim,Jayho Han,Haekyung Lee,Jayoung Kim,Dong Soo Yu,Young Bok Lee
10.17966/JMI.2025.30.2.71 Epub 2025 July 01
Abstract
Onychomycosis is a prevalent fungal infection of the nail apparatus, predominantly caused by dermatophytes. However, nondermatophytic molds, while less common, represent an increasingly recognized etiological group. Among these, Aspergillus, Scopulariopsis, Neoscytalidium, and Fusarium species are frequently implicated. Advancements in molecular diagnostic techniques have facilitated the identification of rare and emerging fungal pathogens implicated in onychomycosis. This case report details the first recorded case of onychomycosis caused by Nothophoma quercina, a fungal species that was previously recognized only as a plant pathogen. A 44-year-old male with severe atopic dermatitis receiving long-term immunosuppressive therapy with cyclosporine and dupilumab developed persistent nail abnormalities. Mycological evaluation, which included potassium hydroxide testing, fungal culture, and molecular analysis, confirmed Nothophoma quercina as the causal organism. The presence of this rare fungus in a human infection underscores the expanding spectrum of nondermatophytic onychomycosis and emphasizes the need to consider atypical pathogens in immunocompromised individuals. The growing use of molecular techniques has facilitated the detection of novel fungal species that may have been previously misidentified or disregarded using conventional methods. This case highlights the need for clinicians to exercise caution while assessing refractory onychomycosis, particularly in high-risk patients. Greater awareness and continued research into rare fungal pathogens will enhance the diagnostic accuracy and developing appropriate antifungal management strategies.
Keywords
Immunosuppression Nondermatophytic molds Nothophoma quercina Onychomycosis Opportunistic fungal infection
Onychomycosis, a fungal infection involving the nail appar- atus, represents one of the most prevalent nail disorders worldwide1, affecting approximately 5~20% of the global population2. This condition is primarily caused by dermato- phytes such as Trichophyton rubrum, T. mentagrophytes, and T. interdigitale3. However, nondermatophytic molds and yeasts also contribute to the prevalence of onychomycosis4, accounting for approximately 20~30% of cases globally5,6. Although less frequently encountered, these uncommon pathogens pose distinct diagnostic challenges and are often associated with underlying risk factors such as immuno- suppression, diabetes, or peripheral vascular diseases7.
This case report details what appears to be the first docu- mented case of Nothophoma quercina-induced onycho- mycosis. The patient, who had severe atopic dermatitis and was receiving long-term immunosuppressive therapy-including biologics such as dupilumab-presented with persistent nail abnormalities. This novel finding emphasizes the significance of including rare pathogens in the differential diagnosis of fungal infections, particularly in vulnerable populations.
A 44-year-old male computer programmer working at a multinational company presented to our clinic with complaints of progressive nail distortion and discoloration. The patient denied any history of sharing footwear or being in close proximity to individuals with similar symptoms. Additionally, he reported no recent travel abroad in the months preceding the onset of his nail-related manifestations.
The patient had a longstanding history of atopic derma- titis (AD), initially diagnosed more than a decade prior to presentation. He had been under regular follow-up at our hospital, where topical tacrolimus was initially used to treat his AD. Despite occasional exacerbations, his symptoms were generally well controlled over time. However, 2 years ago, his AD markedly deteriorated, manifesting as extensive eczema- tous plaques and severe pruritus, which prompted the initi- ation of systemic cyclosporine therapy. Although cyclosporine initially provided symptom relief, his disease flared repeatedly, necessitating multiple intermittent ("stop-and-go") treatment cycles. Given the persistence of refractory symptoms despite cyclosporine therapy, treatment was escalated to include dupilumab.
At the time of dupilumab initiation, the patient's Eczema Area and Severity Index (EASI) score was 36.9, consistent with severe disease. After receiving dupilumab therapy for 16 months, his condition improved substantially, and the EASI score decreased to 3.0. However, during this period of clinical improvement, he developed chronic nail abnormalities-including thickening, discoloration, and a roughened surface texture—which progressively worsened (Fig. 1).

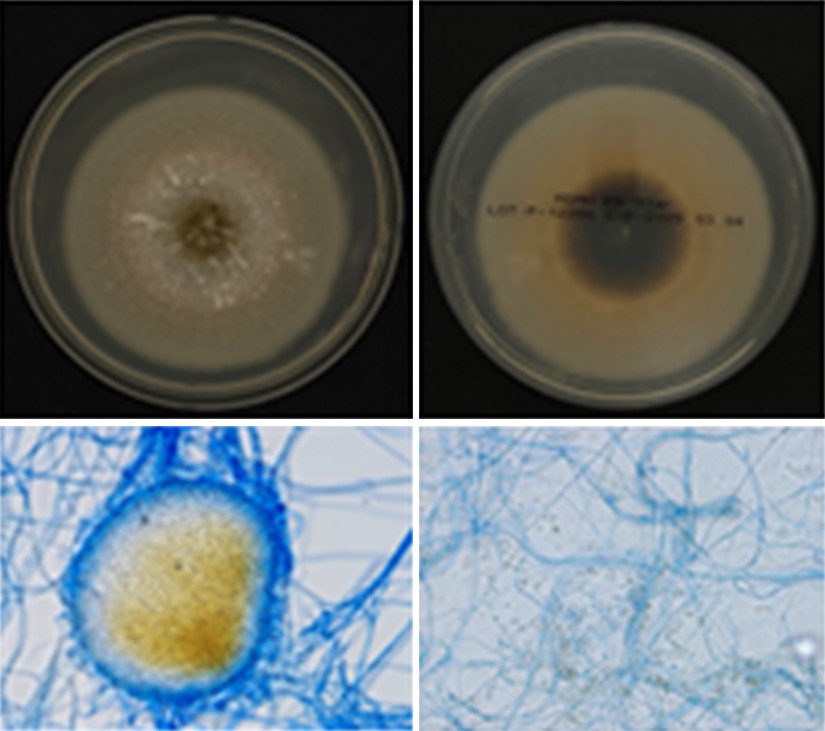
The potassium hydroxide (KOH) test performed on nail scrapings returned a positive result, confirming a fungal in- fection. To identify the specific fungal species, a fungal culture was performed. The fungal isolate obtained from the patient's nail was initially cultured on Sabouraud dextrose agar at 25℃ for 14 days. To obtain a pure culture, the isolate was subcultured onto potato dextrose agar (PDA) and incubated at 25℃. After 10 days of incubation, the colonies developed dull white aerial mycelium with a floccose to downy texture, a greenish-olivaceous surface near the center, and a reverse side with a dark center and a white margin. Microscopic examination of PDA-cultured colonies stained with lactophenol cotton blue revealed the septate, branching, and colorless mycelium passing into conidiophores, black pycnidium. Conidia originating from pycnidia were aseptate, smooth-walled, hyaline to brown in color, and subglobose to oval (Fig. 2).
Molecular identification of the fungal isolate was performed through sequence analysis of the RNA polymerase II second largest subunit (RPB2) and BENA (β-tubulin) genes. Phylo- genetic placement of the isolate was determined by con- structing a maximum likelihood (ML) phylogenetic tree using RPB2 and BENA sequences. These sequences were compared with GenBank entries using BLAST analysis. Pairwise alignment demonstrated a high degree of sequence similarity between the clinical isolate and CBS 633.92, with 259 out of 261 bp identical (99.2%) for the β-tubulin gene and 519 out of 524 bp identical (99.0%) for the RPB2 gene. Phylogenetic analysis conducted with MEGA 6 software provided strong molecular evidence that the clinical isolate was most closely related to Nothophoma quercina CBS 633.92, confirming its species-level identification. This species had never previously been documented as a human pathogen, making this the first reported case of onychomycosis attributed to this fungus. Given the patient's history of immunosuppressive therapy, this rare fungal infection was considered opportunistic.
The patient was prescribed topical efinaconazole (Jublia®), an antifungal agent considered effective against nondermato- phytic molds. However, despite daily application for over a year, complete resolution was not achieved. Given that the infection was recalcitrant, surgical removal of the infected nail was recommended; however, the patient opted to continue topical treatment and declined surgical intervention.
In recent decades, nondermatophytic mold-induced onycho- mycosis has become more prevalent. While dermatophytes remain the primary causative agents, non-dermatophyte molds are increasingly being recognized as significant pathogens, particularly in patients with underlying risk factors such as immunosuppression, chronic dermatologic conditions, and peripheral vascular compromise5. Our patient had several predisposing factors-including long-standing atopic dermatitis and prolonged immunosuppressive therapy with cyclosporine and dupilumab—which placed him at an increased risk for opportunistic fungal infections.
Among nondermatophytic molds, Aspergillus species account for over 50% of global cases8, followed by Scopulari- opsis, Neoscytalidium, and Fusarium, with regional variations9. The spectrum of fungi implicated in onychomycosis has expanded with the identification of several uncommon fungal pathogens.
Originally being described as Cicinobolus quercinus, Nothophoma quercina was subsequently reclassified under Ampelomyces and Phoma before being reassigned to its current designation in 2015 based on phylogenetic analysis10,11. Primarily known as a plant pathogen affecting Quercus species12, it has also been isolated from a human superficial foot lesion13, suggesting its potential as an opportunistic pathogen, particularly in immunocompromised individuals. Notably, Phoma macrostoma, a related species in the Didymellaceae family, has been linked to nondermatophytic onychomycosis14, further supporting the possibility that Notho- phoma species are opportunistic pathogens.
Repeat cultures and molecular identifications were carried out to address the potential for contamination, and N. quercina was consistently identified. Although histopath- ological examination was not performed due to the absence of a biopsy specimen, the identification of N. quercina—a fungus not typically found as a commensal in the human nail microbiota and rarely encountered as a laboratory contaminant-strongly supports its clinical relevance in this case.
Since this is the first reported human case of Nothophoma quercina infection, there is no established treatment regimen. In this case, we applied a regimen typically employed for nondermatophytic mold infections-topical efinaconazole-administered for over a year. However, clinical improvement was limited, and complete resolution was not attained. This outcome implies that N. quercina may exhibit reduced susceptibility to standard topical antifungal agents. In the absence of clinical guidelines, management decisions must rely on the principles established for other nondermatophytic molds, including prolonged topical therapy, systemic agents, and surgical debridement when indicated.
Advancements in molecular diagnostics and fungal taxonomy have enhanced the identification of rare fungal species. Molecular tools now enable the detection of novel pathogens that may have been missed by conventional methods. As fungal taxonomy evolves, clinicians must stay informed of emerging pathogens to enhance the diagnostic accuracy and improve patient outcomes in fungal infections.
This case report presents the first documented case of onychomycosis caused by Nothophoma quercina, a fungal species previously recognized as a plant pathogen. The patient diagnosed with severe atopic dermatitis and undergoing long-term immunosuppressive therapy, developed chronic nail abnormalities, which culminated in the identification of this rare pathogen. The rising incidence of nondermatophytic onychomycosis emphasizes the need for clinicians to consider atypical fungal infections, particularly in immunocompromised individuals. Molecular diagnostic advancements have been instrumental in detecting emerging fungal pathogens, enabling more accurate diagnoses and broadening our under- standing of fungal diversity. As fungal taxonomy continues to evolve, ongoing research and heightened clinical awareness are essential to improve diagnostic precision and optimize treatment strategies for rare fungal infections.
References
1. Piraccini BM, Alessandrini A. Onychomycosis: A review. J Fungi (Basel) 2015;1:30-43
Google Scholar
2. Thomas J, Jacobson GA, Narkowicz CK, Peterson GM, Burnet H, Sharpe C. Toenail onychomycosis: an important global disease burden. J Clin Pharm Ther 2010;35:497-519
Google Scholar
3. Leung AKC, Lam JM, Leong KF, Hon KL, Barankin B, Leung AAM, et al. Onychomycosis: An updated review. Recent Pat Inflamm Allergy Drug Discov 2020;14:32-45
Google Scholar
4. Gupta AK, Ryder JE, Baran R, Summerbell RC. Non-dermatophyte onychomycosis. Dermatol Clin 2003;21: 257-268
Google Scholar
5. Gupta AK, Drummond-Main C, Cooper EA, Brintnell W, Piraccini BM, Tosti A. Systematic review of nondermato- phyte mold onychomycosis: diagnosis, clinical types, epidemiology, and treatment. J Am Acad Dermatol 2012; 66:494-502
Google Scholar
6. Reinel D. Non-dermatophyte fungi in onychomycosis-epidemiology and consequences for clinical practice. Mycoses 2021;64:694-700
Google Scholar
7. Scher RK, Rich P, Pariser D, Elewski B. The epidemiology, etiology, and pathophysiology of onychomycosis. Semin Cutan Med Surg 2013;32:S2-4
Google Scholar
8. Bongomin F, Batac CR, Richardson MD, Denning DW. A review of onychomycosis due to Aspergillus species. Mycopathologia 2018;183:485-493
Google Scholar
9. Noguchi H, Matsumoto T, Kimura U, Hiruma M, Kano R, Yaguchi T, et al. Non-dermatophyte mould onycho- mycosis in Japan. Med Mycol J 2020;61:23-31
Google Scholar
10. Aveskamp MM, de Gruyter J, Woudenberg JH, Verkley GJ, Crous PW. Highlights of the Didymellaceae: A polyphasic approach to characterise Phoma and related pleosporalean genera. Stud Mycol 2010;65:1-60
Google Scholar
11. Xu X, Guo L, Yang C, Teng H, Shen G, Wang S, et al. Diversity and pathogenicity of fungi associated with fruit rot of winter jujube in Shandong Province, China. Plant Dis 2023;107:794-801
Google Scholar
12. Zou J, Dong Y, Wang H, Liang W, Li D. Identification and characterization of Nothophoma quercina causing bud blight on Photinia x fraseri in China. Plant Dis 2021; 105:1356-1364
Google Scholar
13. Valenzuela-Lopez N, Cano-Lira JF, Guarro J, Sutton DA, Wiederhold N, Crous PW, et al. Coelomycetous Dothideomycetes with emphasis on the families Cucur- bitariaceae and Didymellaceae. Stud Mycol 2018;90:1-69
Google Scholar
14. Kukhar E, Smagulova A, Kiyan V. Biological properties of Phoma macrostoma related to non-dermatophyte onychomycosis. Med Mycol Case Rep 2020;27:55-58
Google Scholar
Congratulatory MessageClick here!