pISSN : 3058-423X eISSN: 3058-4302
Open Access, Peer-reviewed

pISSN : 3058-423X eISSN: 3058-4302
Open Access, Peer-reviewed
Jin Ho Kim,Yong Hyun Jang,Seok-Jong Lee
10.17966/JMI.2023.28.2.54 Epub 2023 July 07
Abstract
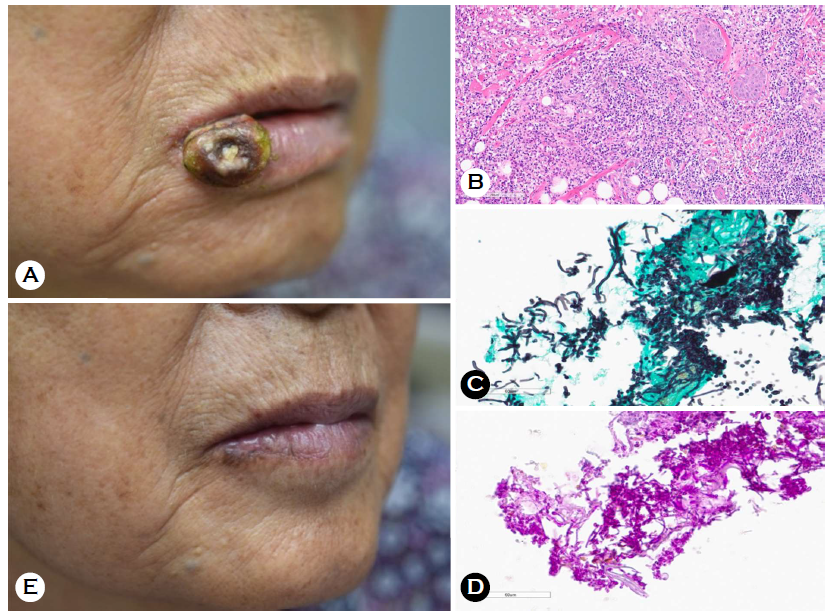
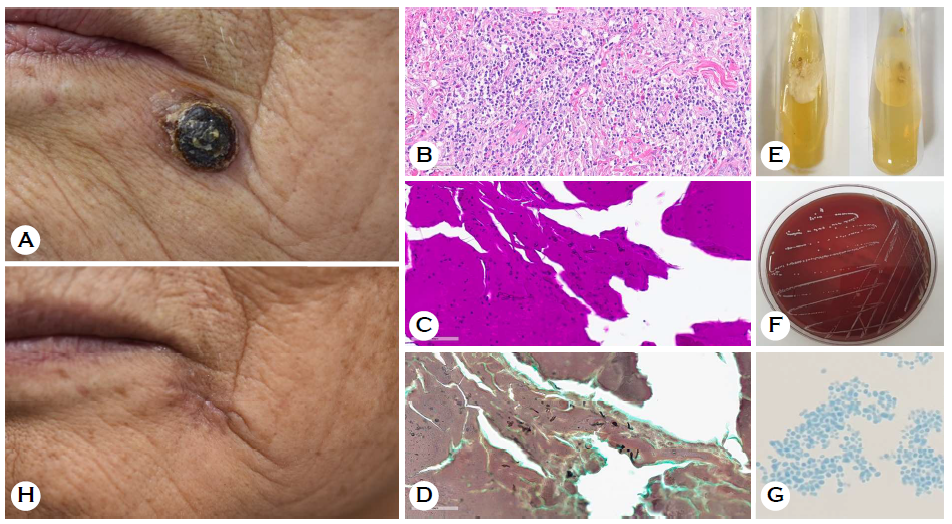
Skin fungal infections are sometimes misdiagnosed as malignancies and vice versa. Herein, we present the case of a 78-year-old woman who visited our clinic because of a rapidly growing "hard-crusted nodule" on the lower lip persisting for 1 month. Keratoacanthoma or squamous cell carcinoma (SCC) was initially considered. However, the histopathological findings revealed suppurative granuloma and fungal elements without atypical cells. Candida albicans was grown in tissue culture. The lesions were treated with topical ketoconazole. After 2 years, the patient revisited because of a black-crusted nodule on the left corner of her mouth that had been persisting for 1 month. The nodule resembled SCC. Histopathological examination revealed suppurative granuloma and fungal elements. After confirming Candida glabrata in fungal culture, the lesion was diagnosed as candidal granuloma and disappeared spontaneously without any treatment. Herein, we report a case of candidal granuloma on lip mimicking recurrent malignancies.
Keywords
Candidal granuloma Fungal infection Malignancy Squamous cell carcinoma
Skin fungal infections, including candidal granuloma, have heterogeneous clinical presentations, including papulo-plaques, nodules, and ulcerative lesions1. They are differentially diagnosed as benign skin lesions and malignant tumors, such as other subcutaneous infections, eczema, squamous cell carcinoma (SCC), fibrolipoma, and Kaposi sarcoma2. Patient burden increases when skin fungal infections are misdiag- nosed as a malignancy as patients are compelled to undergo excessive surgical treatment. Herein, we report a case of candidal granuloma on the lip masquerading as SCC.
A 78-year-old woman presented to our clinic with a solitary and rapidly growing, large bean-sized, hard-crusted, dusky erythematous nodule on the right corner of her lower lip persisting for 1 month (Fig. 1A). The lesion emerged after a minor trauma that occurred while toothbrushing. She had received chemotherapy with dacarbazine for malignant melanoma 10 years ago. Owing to the initial impression of keratoacanthoma or SCC, incisional biopsy was performed. Hematoxylin and eosin (H&E) staining revealed suppurative granuloma with dense neutrophils, histiocytes, and some multinucleated giant cells in the dermis. However, atypical cells were not observed (Fig. 1B). To determine the causes of in- fections rather than the possibility for malignancy, the periodic acid-Schiff with diastase (D-PAS) and Grocott's methenamine silver (GMS) staining were performed. These methods revealed the presence of pinkish yeasts with pseudohyphae (Figs. 1C and D). Candida albicans was identified in fungal culture. Therefore, the lesion was ultimately diagnosed as candidal granuloma. After treatment with topical ketoconazole for 2 weeks, the lesion slowly disappeared (Fig. 1E). After 2 years, the patient presented again with similar black-crusted nodule on the lower left corner of her mouth that had been persisting for 1 month (Fig. 2A). To differentiate between the SCC and candidal granuloma, fungal culture and incisional biopsy with D-PAS and GMS stain were performed. Histopathological examination revealed yeasts measuring 2~3 μm with numer- ous neutrophilic and histiocytic infiltration and the absence of atypical cells (Figs. 2B-D). Fungal culture on both Sabouraud dextrose agar and sheep blood agar revealed smooth and glabrous colonies with a white to cream color (Figs. 2E and F). Ovoid budding blastoconidia measuring 2~3 μm without pseudohyphae were observed in the lactophenol cotton blue stain (Fig. 2G). Candida glabrata was identified in fungal culture. Therefore, the recurring lesion was diagnosed as candidal granuloma, which disappeared spontaneously after 2 weeks (Fig. 2H).
Candidal granuloma is a rare form of mucocutaneous candidiasis usually reported in patients who are immunocompromised. The histopathological findings of such patients are characterized by the neutrophilic and histiocytic inflam- matory reaction expanding into the dermis and formation of suppurative granuloma3. Candidal granuloma is presented as inflammatory papules, nodules and plaques covered with thick crust on face, scalp, and oral mucosa4.
According to the case reports reporting that subcutaneous candidal infection can be misdiagnosed as SCC, cutaneous candidal infections, such as candidal granuloma, are differen- tially diagnosed as malignant tumors, especially SCC5,6. The clinical manifestations presented as inflammatory papules, nodules with hyperkeratosis on face share similarities with SCC. Moreover, the regional lymphadenopathy accompanying candidal infection can be misdiagnosed as malignant lymph node metastasis.
In addition to the symptomatic similarities, the patient's immunocompromised state can be another reason for con- fusing fungal infections with malignancies. Patients who are immunocompromised patients have huge concerns regarding fungal infections and are at an increased risk of skin cancer. It is well known that iatrogenic immunosuppression can lead to an increased risk of secondary or primary tumors, particularly SCC. Kidney and heart transplant patients receiving immunosuppressive therapy have a 65-250-fold increased risk of developing SCC7.
While many modalities can be used to diagnose candidal granuloma, the most definite tool directly relies on micro- scopic examination of hyphae or filaments and isolation of etiologic organism via fungal culture. Histopathological ex- aminations followed by D-PAS and GMS staining revealed neutrophilic and histiocytic infiltration and allow visualization of fungal elements. Although fungal culture is a powerful diagnostic tool for confirming fungal infection, it is not routinely done when malignancy is considered as the initial diagnosis. In a retrospective review of subcutaneous fungal infections in Taiwan, 30% of patients were not initially diag- nosed with fungal infection1 instead with different diseases. Fungal culture was performed in only 36% of the patients.
Although skin fungal infection can be treated with topical or systemic antifungal agents, confusing it with malignancy can result in overtreatment. In a case reported by Efared et al., the patient who had a final diagnosis of fungal infection was amputated to acquire sufficient safety margin due to the initial impression of invasive Kaposi sarcoma8. From this case, it can be concluded that misdiagnosis of skin fungal infection as malignancy increases patient burden as the latter requires more aggressive diagnostic or therapeutic treatment.
In conclusion, we reported a case of candidal granuloma on the lip that was initially diagnosed as a malignancy with clinical manifestation. Thus, we need to be aware that fungal infections in the skin can be misdiagnosed as malignancies, compelling the overtreatment of patient before the con- firmation of the malignancies.
References
1. Hsu TJ, Lee CH. Implantation mycoses and invasive fungal infections with cutaneous involvement in tropical Taiwan: an 11-year retrospective study of a medical center. J Fungi 2023;9:322
Google Scholar
2. Momin SB, Richardson BS, Bryan MG, Del Rosso JQ, Mobini N. Mycetoma clinically masquerading as squa- mous cell carcinoma: case report and literature review. J Clin Aesthet Dermatol 2009;2:26-31
Google Scholar
3. Eom JY, Kim NI, Sim WY, Haw CR. Candida granuloma. Ann Dermatol 1994;6:174-178
4. Anjaneyan G, Gowda V, Kumar A, Eapen M. Candidal granuloma in a renal allograft recipient. Indian J Dermatol Venereol and Leprol 2023;89:99-102
Google Scholar
5. Kim JS, Shin JM, Lee KW, Kim YS, Rao B, Lee Y. Kaposi sarcoma-like lesions caused by Candida guilliermondii infection in a kidney transplant patient. Ann Dermtol 2021;33:91-93
Google Scholar
6. Brothers RP, Daveluy SD. Squamous cell carcinoma mimicking fungal infection. ID Cases 2016;6:72-73
Google Scholar
7. Jensen P, Møller B, Hanse S. Skin cancer in kidney and heart transplant recipients and different long-term immu- nosuppresive therapy regimens. J Am Acad Dermatol 2000;42:307
Google Scholar
8. Efared B, Tahiri L, Boubacar MS, Atsam-Ebang G, Hammas N, Hinde EF, et al. Mycetoma in a non-endemic area: a diagnostic challenge. BMC Clin Pathol 2017;17:1
Google Scholar
Congratulatory MessageClick here!